Per FDA guidelines recommending that manufacturers limit the dose of acetaminophen in prescription products, the formulation of fioricet has changed. “Old formulations” of fioricet contained 50 mg of butalbital, 325 mg of acetaminophen and 40 mg caffeine; “new formulations” contain 50 mg of butalbital, 300 mg of acetaminophen and 40 mg caffeine.
Manufacturers were allowed to make the “old formulation” of fioricet until January 1, 2014. Currently there is no move to remove or destroy the “old formulation”, allowing for an odd situation in which there could be two different formulations of fioricet in pharmacies.
| Formulation | DEA Schedule | Butalbital (mg) | Acetaminophen (mg) | Caffeine (mg) | Form |
|---|---|---|---|---|---|
| Old fioricet | none | 50 | 325 | 40 | tablet |
| New fioricet | CIII | 50 | 300 | 40 | capsule |
CLASSES
Analgesics with Antipyretic Activity Combinations
Opioid Agonists and Other Drug Combinations
DEA CLASS
Rx, schedule III
DESCRIPTION
Acetaminophen, barbiturate (butalbital), and caffeine analgesic combination
Used to treat tension headaches in adult and pediatric patients 12 years and older; extended use not advisable
Associated with concerns of abuse, medication-overuse headache, and withdrawal; boxed warning for acetaminophen hepatotoxicity risk
COMMON BRAND NAMES
Alagesic, Americet, Anolor-300, Arcet, BAC, CAPACET, Esgic, Ezol, Fioricet, Geone, Margesic, Medigesic, Orbivan, Pacaps, Phrenilin Forte, Repan, Tenake, Triad, Vanatol LQ, Vanatol S, Zebutal
HOW SUPPLIED
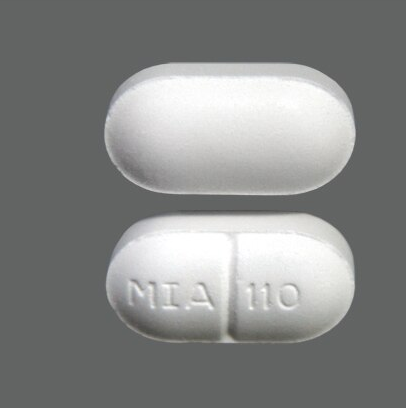
Alagesic/Anolor-300/Arcet/Butalbital, Acetaminophen, Caffeine/CAPACET/Esgic/Ezol/Fioricet/Geone/Margesic/Medigesic/Orbivan/Pacaps/Phrenilin Forte/Tenake/Triad/Zebutal Oral Cap: 50-300-40mg, 50-325-40mg
Americet/BAC/Butalbital, Acetaminophen, Caffeine/Esgic/Fioricet/Repan Oral Tab: 50-325-40mg
Vanatol LQ/Vanatol S Oral Liq: 15mL, 50-325-40mg
DOSAGE & INDICATIONS
1 to 2 tablets or capsules PO every 4 hours as needed. Do not exceed 6 tablets or capsules in a 24-hour period.
15 mL to 30 mL PO every 4 hours as needed. Do not exceed 90 mL in a 24-hour period.
15 mL to 30 mL PO every 4 hours as needed. Do not exceed 90 mL in a 24-hour period.
†Indicates off-label use
MAXIMUM DOSAGE
Acetaminophen 4 grams/day PO, caffeine 240 mg/day PO, or butalbital 300 mg/day PO.
Acetaminophen 4 grams/day PO, caffeine 240 mg/day PO, or butalbital 300 mg/day PO.
Acetaminophen 4 grams/day PO, caffeine 240 mg/day PO, or butalbital 300 mg/day PO.
12 years: Acetaminophen 4 grams/day PO, caffeine 240 mg/day PO, or butalbital 300 mg/day PO.
Less than 12 years: Safety and efficacy have not been established.
Safety and efficacy have not been established.
DOSING CONSIDERATIONS
Acetaminophen should be used with extreme caution in patients with impaired hepatic function or with a history of overdose. Acetaminophen should not be used in patients with a history of alcoholism. Patients with stable hepatic disease may receive therapeutic doses of acetaminophen for episodic pain of short duration (< 5 days).
Dosage should be modified depending on clinical response and degree of renal impairment, but no quantitative recommendations are available.
STORAGE
Alagesic:
– Store at controlled room temperature (between 68 and 77 degrees F)
Alagesic LQ:
– Store at controlled room temperature (between 68 and 77 degrees F)
Americet:
– Store at controlled room temperature (between 68 and 77 degrees F)
Anolor-300:
– Store at controlled room temperature (between 68 and 77 degrees F)
Arcet :
– Store at controlled room temperature (between 68 and 77 degrees F)
BAC :
– Store at controlled room temperature (between 68 and 77 degrees F)
CAPACET:
– Store at controlled room temperature (between 68 and 77 degrees F)
Dolgic Plus:
– Store at controlled room temperature (between 68 and 77 degrees F)
Esgic:
– Store at controlled room temperature (between 68 and 77 degrees F)
Esgic Plus:
– Store at controlled room temperature (between 68 and 77 degrees F)
Ezol:
– Store at controlled room temperature (between 68 and 77 degrees F)
Fioricet:
– Store at controlled room temperature (between 68 and 77 degrees F)
Geone:
– Store at controlled room temperature (between 68 and 77 degrees F)
Margesic:
– Store at controlled room temperature (between 68 and 77 degrees F)
Medigesic:
– Store at controlled room temperature (between 68 and 77 degrees F)
Orbivan :
– Store at controlled room temperature (between 68 and 77 degrees F)
Pacaps :
– Store at controlled room temperature (between 68 and 77 degrees F)
Phrenilin Forte:
– Store at controlled room temperature (between 68 and 77 degrees F)
Repan:
– Store at controlled room temperature (between 68 and 77 degrees F)
Tenake :
– Store at controlled room temperature (between 68 and 77 degrees F)
Triad:
– Store at controlled room temperature (between 68 and 77 degrees F)
Vanatol LQ:
– Store at controlled room temperature (between 68 and 77 degrees F)
Vanatol S:
– Store at controlled room temperature (between 68 and 77 degrees F)
Zebutal:
– Store at controlled room temperature (between 68 and 77 degrees F)
CONTRAINDICATIONS / PRECAUTIONS
NOTE: This monograph discusses the use of acetaminophen; butalbital; caffeine combination products. Clinicians may wish to consult the individual monographs for more information about the specific contraindications and precautions for each agent.
Acetaminophen; butalbital; caffeine is contraindicated in patients with acetaminophen hypersensitivity, barbiturate hypersensitivity, or hypersensitivity to any of the other product components. Acetaminophen hypersensitivity reactions are rare, but severe sensitivity reactions are possible. Barbiturates can cause severe and potentially fatal reactions that are preceded by skin eruptions. Therapy should be prescribed only after critical benefit-to-risk appraisal in patients with a history of adverse hematologic response (i.e., agranulocytosis), hypersensitivity, or other adverse reactions to barbiturates or other anticonvulsants. Skin reactions can precede potentially fatal hypersensitivity reactions; exfoliative dermatitis has resulted in fatalities. Hypersensitivity reactions have been reported in patients who previously experienced hydantoin hypersensitivity (e.g., phenytoin) or carbamazepine hypersensitivity. Estimates of cross-sensitivity vary, but may range from 30—80%. There is no way to predict with certainty which patients will exhibit cross-sensitivity.
Acetaminophen; butalbital; caffeine is contraindicated in patients with porphyria as use may trigger symptoms of the disease. Barbiturates can stimulate the accumulation of porphyrin precursors.
Acetaminophen; butalbital; caffeine should be used with caution in patients with mental status changes such as major depression or suicidal ideation due to exacerbation of these conditions by the CNS depressant effects of butalbital. Caffeine should be prescribed cautiously to certain high risk patients such as older adult or debilitated patients or patients with cardiac disease because of possible effects on heart rate or blood pressure in higher daily doses.
Acetaminophen; butalbital; caffeine has the potential for overdose or poisoning; overdose of acetaminophen may cause hepatotoxicity and acute liver failure, at times resulting in liver transplant and death. Most cases of liver injury are associated with the use of acetaminophen at doses exceeding 4 grams per day and often involve the use of more than one acetaminophen-containing product. Advise patients and caregivers to carefully read nonprescription (OTC) and prescription labels, to avoid excessive and/or duplicate medications, and to seek medical help immediately if more than 4 grams of acetaminophen is ingested in 1 day, even if they feel well. The risk of acute liver failure is high in individuals with underlying hepatic disease and in individuals who ingest alcohol while taking acetaminophen. Use acetaminophen; butalbital; caffeine with caution, if at all, in patients with pre-existing hepatic disease (e.g., alcoholic hepatic disease or viral hepatitis). Patients who drink more than 3 alcoholic drinks a day and take acetaminophen are at increased risk of developing hepatotoxicity. Administration of this product should be limited or avoided altogether in patients with alcoholism or patients who consume alcohol regularly due to the increased risk for hepatotoxicity; alcohol use also increases the risk for CNS and respiratory depression from the butalbital in this drug product. Hepatically-impaired patients may require lower dosage and slower dosage titration of the components of this drug combination; in general, avoid use in patients with severe liver impairment. Because barbiturates may impair the ability of the liver to metabolize ammonia, barbiturates are best avoided in patients with hepatic encephalopathy. Note that barbiturates are hepatic enzyme inducers and patients should be monitored for altered drug levels and therapeutic effects as indicated. Liver function tests may need to be monitored.
Because butalbital can cause dose-dependent respiratory depression, it should be used cautiously in patients with pulmonary disease states causing respiratory depression, dyspnea, severe pulmonary insufficiency or airway obstruction. Barbiturates should be avoided in patients with bronchopneumonia. Use with close supervision in patients with sleep apnea or chronic obstructive pulmonary disease (COPD). Avoid butalbital use in patients with status asthmaticus or asthma.
Acetaminophen; butalbital; caffeine may cause blurred vision, drowsiness, or dizziness, especially with initial use. Advise patients to use caution when driving or operating machinery until they are aware of the effects of the drug. Like all barbiturates, butalbital may cause CNS depression. Because butalbital can cause drowsiness and a decreased level of consciousness, there is a higher risk of falls, particularly in the elderly, with the potential for subsequent severe injuries. CNS depressant effects are increased during coadministration with other CNS depressants, including alcohol. Avoid ethanol ingestion during the use of barbiturates due to the potential for additive CNS depressant effects; the lethal dose of a barbiturate is significantly less if alcohol is also ingested. Ethanol intoxication must be avoided. Additionally, acetaminophen should not be used in patients who consume 3 or more alcoholic beverages per day due to a potential increased risk of drug-induced hepatotoxicity. Use of this drug product in patients with alcoholism is not advisable.
In general, use acetaminophen; butalbital; caffeine with caution in those patients with acute abdomen conditions or with severe renal impairment or renal failure.
Acetaminophen; butalbital; caffeine combinations are classified as FDA pregnancy-risk category C and should be used during pregnancy only if the benefits to the mother outweigh the potential risks to the fetus. All three components cross the placenta. There have been reports of physical abnormalities in infants correlating to exposure to barbiturates in utero. Additionally, a retrospective study revealed that in utero exposure to barbiturates was associated with intelligence deficits. Repeated use of butalbital during the third trimester can also cause physical dependence in the neonate. A withdrawal seizure has been reported in a 2-day old infant whose mother had been taking a butalbital-containing medication during the last 2 months of her pregnancy. If the mother used butalbital late in pregnancy, newborns should also be carefully observed for signs of ventilatory depression, particularly if the infant is premature. There is no established use for butalbital during labor or obstetrical delivery. Neonatal arrhythmias (e.g., tachycardia, premature atrial contractions) and tachypnea have been reported when caffeine was consumed during pregnancy in amounts > 500 mg/day. Caffeine withdrawal in the neonate after birth may account for these symptoms. Fatal arrhythmias in neonates with caffeine use by the mother have also been reported. Females should be warned of the potential adverse effects on the fetus should pregnancy occur while taking acetaminophen-butalbital-caffeine combinations.
Acetaminophen; butalbital; caffeine components may all be excreted to some extent into breast milk. According to the manufacturer, because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug. Caffeine can accumulate in the neonate. Chronic barbiturate use while breast-feeding may cause dependence in the neonate. The chronic use of acetaminophen; butalbital; caffeine during breast-feeding is not recommended. Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breast-feeding infant experiences an adverse effect related to a maternally ingested drug, healthcare providers are encouraged to report the adverse effect to the FDA.
The safety and efficacy of acetaminophen; butalbital; caffeine combinations have not been established in children.
Symptoms of acute infection (e.g., fever, pain) can be masked during treatment with acetaminophen in patients with bone marrow suppression or immunosuppression.
Acetaminophen; butalbital; caffeine combinations should be prescribed with caution to patients with known substance abuse because of the potential for psychological and/or physical dependence to butalbital. Avoid abrupt discontinuation of butalbital after prolonged use to limit drug withdrawal and/or seizure onset. Sudden, abrupt discontinuation of butalbital in epileptic patients may precipitate acute seizures, status epilepticus, or other seizure disorder.
Patients taking warfarin (Coumadin) anticoagulant therapy may not be appropriate candidates for acetaminophen; butalbital (see Drug Interactions).
Acetaminophen; butalbital; caffeine should be used with caution in geriatric patients due to sensitivity to the CNS and respiratory depressant effects of butalbital; use care in dosage selection. Because butalbital can cause drowsiness and a decreased level of consciousness, there is a higher risk of falls, particularly in the elderly, with the potential for subsequent severe injuries. Butalbital is known to be substantially excreted by the kidney. Because elderly patients are more likely to have decreased renal function, it may be useful to monitor renal function. According to the Beers Criteria, barbiturates are considered potentially inappropriate medications (PIMs) in geriatric patients and should be avoided due to the high rate of physical dependence, tolerance to sedative effects, and risk of overdose at low dosages. The federal Omnibus Budget Reconciliation Act (OBRA) regulates medication use in residents of long-term care facilities (LTCFs); barbiturates generally should not be used since they are highly addictive and can cause multiple adverse effects in the elderly and may increase the metabolism of other necessary chronic medications and lessen their effectiveness.
Patients with G6PD deficiency who overdose with acetaminophen may be at increased risk for drug-induced hemolysis. During acetaminophen overdose, cyanosis may not be apparent in patients with preexisting anemia, in spite of dangerously high blood concentrations of methemoglobin.
ADVERSE REACTIONS
hepatic necrosis / Delayed / Incidence not known
renal papillary necrosis / Delayed / Incidence not known
interstitial nephritis / Delayed / Incidence not known
renal failure (unspecified) / Delayed / Incidence not known
renal tubular necrosis / Delayed / Incidence not known
methemoglobinemia / Early / Incidence not known
pancytopenia / Delayed / Incidence not known
hemolytic anemia / Delayed / Incidence not known
agranulocytosis / Delayed / Incidence not known
angioedema / Rapid / Incidence not known
acute generalized exanthematous pustulosis (AGEP) / Delayed / Incidence not known
anaphylactoid reactions / Rapid / Incidence not known
toxic epidermal necrolysis / Delayed / Incidence not known
erythema multiforme / Delayed / Incidence not known
exfoliative dermatitis / Delayed / Incidence not known
seizures / Delayed / Incidence not known
elevated hepatic enzymes / Delayed / Incidence not known
encephalopathy / Delayed / Incidence not known
hypoprothrombinemia / Delayed / Incidence not known
constipation / Delayed / Incidence not known
hyperglycemia / Delayed / Incidence not known
dysphagia / Delayed / Incidence not known
jaundice / Delayed / Incidence not known
thrombocytosis / Delayed / Incidence not known
neutropenia / Delayed / Incidence not known
hemolysis / Early / Incidence not known
thrombocytopenia / Delayed / Incidence not known
edema / Delayed / Incidence not known
contact dermatitis / Delayed / Incidence not known
erythema / Early / Incidence not known
tolerance / Delayed / Incidence not known
euphoria / Early / Incidence not known
confusion / Early / Incidence not known
hot flashes / Early / Incidence not known
depression / Delayed / Incidence not known
palpitations / Early / Incidence not known
sinus tachycardia / Rapid / Incidence not known
physiological dependence / Delayed / Incidence not known
withdrawal / Early / Incidence not known
psychological dependence / Delayed / Incidence not known
dyspnea / Early / Incidence not known
nausea / Early / Incidence not known
dyspepsia / Early / Incidence not known
vomiting / Early / Incidence not known
abdominal pain / Early / Incidence not known
anorexia / Delayed / Incidence not known
flatulence / Early / Incidence not known
xerostomia / Early / Incidence not known
polyuria / Early / Incidence not known
increased urinary frequency / Early / Incidence not known
purpura / Delayed / Incidence not known
fever / Early / Incidence not known
urticaria / Rapid / Incidence not known
photosensitivity / Delayed / Incidence not known
acneiform rash / Delayed / Incidence not known
rash / Early / Incidence not known
maculopapular rash / Early / Incidence not known
pruritus / Rapid / Incidence not known
agitation / Early / Incidence not known
drowsiness / Early / Incidence not known
vertigo / Early / Incidence not known
irritability / Delayed / Incidence not known
lethargy / Early / Incidence not known
anxiety / Delayed / Incidence not known
syncope / Early / Incidence not known
dizziness / Early / Incidence not known
paresthesias / Delayed / Incidence not known
tremor / Early / Incidence not known
insomnia / Early / Incidence not known
ptosis / Delayed / Incidence not known
headache / Early / Incidence not known
nasal congestion / Early / Incidence not known
hyperhidrosis / Delayed / Incidence not known
fatigue / Early / Incidence not known
musculoskeletal pain / Early / Incidence not known
tinnitus / Delayed / Incidence not known
otalgia / Early / Incidence not known
DRUG INTERACTIONS
Abacavir; Lamivudine, 3TC; Zidovudine, ZDV: (Minor) Both acetaminophen and zidovudine, ZDV undergo glucuronidation. Competition for the metabolic pathway is thought to have caused a case of acetaminophen-related hepatotoxicity. This interaction may be more clinically significant in patients with depleted glutathione stores, such as patients with acquired immunodeficiency syndrome, poor nutrition, or alcoholism.
Abemaciclib: (Major) Avoid coadministration of butalbital with abemaciclib due to decreased exposure to abemaciclib and its active metabolites, which may lead to reduced efficacy. Consider alternative treatments. Abemaciclib is a CYP3A4 substrate and butalbital is a moderate CYP3A4 inducer. Coadministration with moderate CYP3A4 inducers is predicted to decrease the relative potency adjusted unbound AUC of abemaciclib plus its active metabolites (M2, M18, and M20) by 53%, 41%, and 29% respectively.
Acetaminophen; Aspirin, ASA; Caffeine: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. High-dose, chronic administration of the combined analgesics significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Acetaminophen; Butalbital: (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Acetaminophen; Butalbital; Caffeine; Codeine: (Major) Concomitant use of codeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when codeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of codeine with a barbiturate can decrease codeine concentrations, resulting in less metabolism by CYP2D6 and decreased morphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of codeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4. Codeine is primarily metabolized by CYP2D6 to morphine, and by CYP3A4 to norcodeine; norcodeine does not have analgesic properties. (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Acetaminophen; Caffeine; Dihydrocodeine: (Major) Concomitant use of dihydrocodeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when dihydrocodeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of dihydrocodeine with a barbiturate can decrease dihydrocodeine concentrations, resulting in less metabolism by CYP2D6 and decreased dihydromorphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of dihydrocodeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4, an isoenzyme partially responsible for the metabolism of dihydrocodeine.
Acetaminophen; Caffeine; Magnesium Salicylate; Phenyltoloxamine: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. Although salicylates are rarely associated with nephrotoxicity, high-dose, chronic administration of salicylates combined other analgesics, including acetaminophen, significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Additive hepatic toxicity may occur, especially in combined overdose situations. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Acetaminophen; Caffeine; Phenyltoloxamine; Salicylamide: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur.
Acetaminophen; Chlorpheniramine; Dextromethorphan; Phenylephrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Acetaminophen; Chlorpheniramine; Dextromethorphan; Pseudoephedrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Acetaminophen; Chlorpheniramine; Phenylephrine; Phenyltoloxamine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Acetaminophen; Codeine: (Major) Concomitant use of codeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when codeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of codeine with a barbiturate can decrease codeine concentrations, resulting in less metabolism by CYP2D6 and decreased morphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of codeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4. Codeine is primarily metabolized by CYP2D6 to morphine, and by CYP3A4 to norcodeine; norcodeine does not have analgesic properties.
Acetaminophen; Dextromethorphan; Doxylamine: (Moderate) Because doxylamine can cause pronounced sedation, an enhanced CNS depressant effect may occur when it is combined with other CNS depressants including anxiolytics, sedatives, and hypnotics, such as barbiturates.
Acetaminophen; Dextromethorphan; Guaifenesin; Phenylephrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Acetaminophen; Dextromethorphan; Phenylephrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Acetaminophen; Dextromethorphan; Pseudoephedrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Acetaminophen; Dichloralphenazone; Isometheptene: (Major) Additive CNS depression may occur if barbiturates are used concomitantly with dichloralphenazone. (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants.
Acetaminophen; Diphenhydramine: (Major) Because diphenhydramine can cause pronounced sedation, an enhanced CNS depressant effect may occur when it is combined with other CNS depressants including anxiolytics, sedatives, and hypnotics, such as barbiturates.
Acetaminophen; Guaifenesin; Phenylephrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Acetaminophen; Hydrocodone: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate.
Acetaminophen; Oxycodone: (Major) Concomitant use of oxycodone with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concurrent use of oxycodone with a barbiturate may decrease oxycodone plasma concentrations, decrease opioid efficacy, and potentially lead to a withdrawal syndrome in those with physical dependence to opioid agonists. Monitor for signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of increased opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; oxycodone is a CYP3A4 substrate.
Acetaminophen; Pentazocine: (Moderate) Concomitant use of pentazocine with other CNS depressants can potentiate respiratory depression, CNS depression, and sedation. Pentazocine should be used cautiously in any patient receiving these agents, which may include barbiturates.
Acetaminophen; Pseudoephedrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Acetaminophen; Tramadol: (Major) Concomitant use of tramadol with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of tramadol with a barbiturate can decrease tramadol concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of tramadol and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of seizures, serotonin syndrome, and the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; tramadol is a CYP3A4 substrate.
Acetazolamide: (Minor) Acetazolamide can induce osteomalacia in patients treated chronically with barbiturates. Potential mechanisms for this interaction include a carbonic anhydrase inhibitor induced increase in the urinary excretion of calcium and an increase in barbiturate effects resulting from metabolic acidosis. Acetazolamide can also increase the rate of excretion of weakly acidic drugs, such as barbiturates.
Aclidinium; Formoterol: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Acrivastine; Pseudoephedrine: (Moderate) Additive CNS depression may occur if barbiturates are used concomitantly with acrivastine. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Adenosine: (Major) Methylxanthines, such as theophylline, aminophylline, or caffeine, competitively block the effects of adenosine. If possible, stop use of methylxanthines at least 5 half-lives prior to administering adenosine. Patients receiving theophylline, aminophylline and adenosine should be monitored for adenosine efficacy; larger doses of adenosine may be required to achieve antiarrhythmic goals in some patients. In addition, larger doses of adenosine may be required for therapeutic effect if administered to patients with high daily caffeine intake (including caffeine from foods and beverages such as coffee, green tea, other teas, colas, and chocolate). Theophylline, aminophylline may increase the risk of seizures associated with adenosine; avoid methylxanthine use in patients who have experienced an adenosine-associated seizure. Methylxanthines, such as caffeine, theophylline, and theobromine, are also found in guarana.
Albuterol: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Albuterol; Ipratropium: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Aldesleukin, IL-2: (Moderate) Aldesleukin, IL-2 may affect CNS function significantly. Therefore, psychotropic pharmacodynamic interactions could occur following concomitant administration of drugs with significant CNS activity. Use with caution.
Alfentanil: (Major) Concomitant use of alfentanil with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concurrent use of alfentanil with a barbiturate may decrease alfentanil plasma concentrations, decrease opioid efficacy, and potentially lead to a withdrawal syndrome in those with physical dependence to opioid agonists. Monitor for signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of increased opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; alfentanil is a CYP3A4 substrate.
Aliskiren; Amlodipine: (Major) Barbiturates may induce the CYP3A4 metabolism of calcium-channel blockers such as amlodipine, and thereby reduce their oral bioavailability. The dosage requirements of amlodipine may be increased in patients receiving concurrent enzyme inducers; monitor blood pressure closely.
Aliskiren; Amlodipine; Hydrochlorothiazide, HCTZ: (Major) Barbiturates may induce the CYP3A4 metabolism of calcium-channel blockers such as amlodipine, and thereby reduce their oral bioavailability. The dosage requirements of amlodipine may be increased in patients receiving concurrent enzyme inducers; monitor blood pressure closely. (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Aliskiren; Hydrochlorothiazide, HCTZ: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Alprazolam: (Moderate) Additive CNS and/or respiratory depression may occur. Additionally, the oral clearance of alprazolam (0.8 mg single dose) was increased in the presence of another CYP3A4 inducer for 10 days from 0.9 +/- 0.21 mL/minute/kg to 2.13 +/- 0.54 mL/minute/kg and the elimination half-life was shortened from 17.1 +/- 4.9 to 7.7 +/- 1.7 hours. Alprazolam is a CYP3A4 substrate. Barbiturates are CYP3A4 inducers.
Altretamine: (Minor) Because altretamine undergoes significant metabolism by the cytochrome P450 system, agents that stimulate CYP450 enzymes, such as barbiturates, increase the metabolism of altretamine and may result in decreased therapeutic effects.
Amantadine: (Major) Amantadine used concomitantly with psychostimulants, such as caffeine, can result in increased stimulant effects, such as nervousness, irritability, or insomnia, and can lead to seizures or cardiac arrhythmias. Close monitoring of the patient is recommended.
Amiloride; Hydrochlorothiazide, HCTZ: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Aminosalicylate sodium, Aminosalicylic acid: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur.
Amiodarone: (Minor) Amiodarone is an inhibitor of CYP1A2 isoenzymes, and could theoretically reduce CYP1A2-mediated caffeine metabolism. The clinical significance of this potential interaction is not known.
Amitriptyline; Chlordiazepoxide: (Moderate) Additive CNS and/or respiratory depression may occur. Additionally, barbiturates may increase the metabolism of chlordiazepoxide. Chlordiazepoxide is a CYP3A4 substrate. Barbiturates are CYP3A4 inducers.
Amlodipine: (Major) Barbiturates may induce the CYP3A4 metabolism of calcium-channel blockers such as amlodipine, and thereby reduce their oral bioavailability. The dosage requirements of amlodipine may be increased in patients receiving concurrent enzyme inducers; monitor blood pressure closely.
Amlodipine; Atorvastatin: (Major) Barbiturates may induce the CYP3A4 metabolism of calcium-channel blockers such as amlodipine, and thereby reduce their oral bioavailability. The dosage requirements of amlodipine may be increased in patients receiving concurrent enzyme inducers; monitor blood pressure closely. (Minor) CYP3A4 inducers like the barbiturates may decrease the efficacy of atorvastatin, a CYP3A4 substrate. Monitor for potential reduced cholesterol-lowering efficacy when these drugs are co-administered.
Amlodipine; Benazepril: (Major) Barbiturates may induce the CYP3A4 metabolism of calcium-channel blockers such as amlodipine, and thereby reduce their oral bioavailability. The dosage requirements of amlodipine may be increased in patients receiving concurrent enzyme inducers; monitor blood pressure closely.
Amlodipine; Hydrochlorothiazide, HCTZ; Olmesartan: (Major) Barbiturates may induce the CYP3A4 metabolism of calcium-channel blockers such as amlodipine, and thereby reduce their oral bioavailability. The dosage requirements of amlodipine may be increased in patients receiving concurrent enzyme inducers; monitor blood pressure closely. (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Amlodipine; Hydrochlorothiazide, HCTZ; Valsartan: (Major) Barbiturates may induce the CYP3A4 metabolism of calcium-channel blockers such as amlodipine, and thereby reduce their oral bioavailability. The dosage requirements of amlodipine may be increased in patients receiving concurrent enzyme inducers; monitor blood pressure closely. (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Amlodipine; Olmesartan: (Major) Barbiturates may induce the CYP3A4 metabolism of calcium-channel blockers such as amlodipine, and thereby reduce their oral bioavailability. The dosage requirements of amlodipine may be increased in patients receiving concurrent enzyme inducers; monitor blood pressure closely.
Amlodipine; Telmisartan: (Major) Barbiturates may induce the CYP3A4 metabolism of calcium-channel blockers such as amlodipine, and thereby reduce their oral bioavailability. The dosage requirements of amlodipine may be increased in patients receiving concurrent enzyme inducers; monitor blood pressure closely.
Amlodipine; Valsartan: (Major) Barbiturates may induce the CYP3A4 metabolism of calcium-channel blockers such as amlodipine, and thereby reduce their oral bioavailability. The dosage requirements of amlodipine may be increased in patients receiving concurrent enzyme inducers; monitor blood pressure closely.
Amobarbital: (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Amoxapine: (Major) Monitor for excessive sedation and somnolence during coadministration of amoxapine and barbiturates. Concurrent use may result in additive CNS depression.
Amoxicillin; Clarithromycin; Lansoprazole: (Moderate) Monitor for decreased efficacy of lansoprazole if concomitant use of lansoprazole and barbiturates is necessary. Lansoprazole is metabolized by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Drugs known to induce CYP3A4 and CYP2C19 may lead to decreased lansoprazole plasma concentrations.
Amoxicillin; Clarithromycin; Omeprazole: (Major) Avoid coadministration of omeprazole with barbiturates because it can result in decreased efficacy of omeprazole. Omeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19.
Amphetamine: (Moderate) Avoid excessive caffeine intake during use of the amphetamine salts. Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants. Excessive caffeine ingestion (via medicines, foods like chocolate, dietary supplements, or beverages including coffee, green tea, other teas, colas) may contribute to side effects like nervousness, irritability, nausea, insomnia, or tremor. Patients should avoid medications and dietary supplements which contain high amounts of caffeine.
Amphetamine; Dextroamphetamine Salts: (Moderate) Avoid excessive caffeine intake during use of the amphetamine salts. Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants. Excessive caffeine ingestion (via medicines, foods like chocolate, dietary supplements, or beverages including coffee, green tea, other teas, colas) may contribute to side effects like nervousness, irritability, nausea, insomnia, or tremor. Patients should avoid medications and dietary supplements which contain high amounts of caffeine.
Amphetamine; Dextroamphetamine: (Moderate) Avoid excessive caffeine intake during use of the amphetamine salts. Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants. Excessive caffeine ingestion (via medicines, foods like chocolate, dietary supplements, or beverages including coffee, green tea, other teas, colas) may contribute to side effects like nervousness, irritability, nausea, insomnia, or tremor. Patients should avoid medications and dietary supplements which contain high amounts of caffeine.
Amprenavir: (Major) Coadministration with phenobarbital and, potentially, other barbiturates may increase the metabolism of amprenavir and lead to decreased amprenavir concentrations resulting in reduction of antiretroviral efficacy and development of viral resistance. If amprenavir and barbiturates are used together, the patient must be closely monitored for antiviral efficacy.
Anagrelide: (Moderate) Anagrelide has been shown to inhibit CYP1A2. In theory, coadministration of anagrelide with substrates of CYP1A2, including caffeine, could lead to increases in the serum concentrations of caffeine and, thus, adverse effects. (Moderate) Anagrelide is partially metabolized by CYP1A2. Coadministration of anagrelide with drugs that induce CYP1A2, such as barbiturates, could theoretically increase the elimination of anagrelide and decrease the efficacy of anagrelide.
Antacids: (Minor) Antacids can delay the oral absorption of acetaminophen, but the interactions are not likely to be clinically significant as the extent of acetaminophen absorption is not appreciably affected.
Apomorphine: (Moderate) Apomorphine causes significant somnolence. Concomitant administration of apomorphine and CNS depressants could result in additive depressant effects.
Apraclonidine: (Minor) No specific drug interactions were identified with systemic agents and apraclonidine during clinical trials. Theoretically, apraclonidine might potentiate the effects of CNS depressant drugs such as the anxiolytics, sedatives, and hypnotics, including barbiturates or benzodiazepines.
Apremilast: (Major) The coadministration of apremilast and barbiturates is not recommended. Apremilast is metabolized primarily by CYP3A4, with minor metabolism by CYP1A2; barbiturates are strong CYP3A4 inducers and also induce CYP1A2. Coadministration of rifampin, another strong CYP3A4 inducer, with a single dose of apremilast resulted in a decrease in apremilast AUC and Cmax by 72% and 43%, respectively. A similar reduction in systemic exposure may be seen with coadministration of apremilast and barbiturates which may result in a loss of efficacy of apremilast.
Aprepitant, Fosaprepitant: (Minor) Use caution if acetaminophen and aprepitant are used concurrently and monitor for an increase in acetaminophen-related adverse effects for several days after administration of a multi-day aprepitant regimen. Acetaminophen is a minor (10 to 15%) substrate of CYP3A4. Aprepitant, when administered as a 3-day oral regimen (125 mg/80 mg/80 mg), is a moderate CYP3A4 inhibitor and inducer and may increase plasma concentrations of acetaminophen. For example, a 5-day oral aprepitant regimen increased the AUC of another CYP3A4 substrate, midazolam (single dose), by 2.3-fold on day 1 and by 3.3-fold on day 5. After a 3-day oral aprepitant regimen, the AUC of midazolam (given on days 1, 4, 8, and 15) increased by 25% on day 4, and then decreased by 19% and 4% on days 8 and 15, respectively. As a single 125 mg or 40 mg oral dose, the inhibitory effect of aprepitant on CYP3A4 is weak, with the AUC of midazolam increased by 1.5-fold and 1.2-fold, respectively. After administration, fosaprepitant is rapidly converted to aprepitant and shares many of the same drug interactions. However, as a single 150 mg intravenous dose, fosaprepitant only weakly inhibits CYP3A4 for a duration of 2 days; there is no evidence of CYP3A4 induction. Fosaprepitant 150 mg IV as a single dose increased the AUC of midazolam (given on days 1 and 4) by approximately 1.8-fold on day 1; there was no effect on day 4. Less than a 2-fold increase in the midazolam AUC is not considered clinically important.
Arformoterol: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Aripiprazole: (Major) Because aripiprazole is metabolized by CYP3A4, the manufacturer recommends that the oral aripiprazole dose be doubled over 1 to 2 weeks when strong CYP3A4 inducers, such as barbiturates, are added to aripiprazole therapy. If these agents are used in combination, the patient should be carefully monitored for a decrease in aripiprazole efficacy. When the CYP3A4 inducer is withdrawn from the combination therapy, the aripiprazole dose in adults should be reduced over 1 to 2 weeks to the original level. Avoid concurrent use of Abilify Maintena with a CYP3A4 inducer when the combined treatment period exceeds 14 days because aripiprazole blood concentrations decline and may become suboptimal. In adults receiving 662 mg, 882 mg, or 1,064 mg of Aristada and receiving a strong CYP3A4 inducer, no dosage adjustment is necessary; however, the 441 mg dose should be increased to 662 mg if the CYP inducer is added for more than 2 weeks. Avoid concurrent use of Aristada Initio and strong CYP3A4 inducers. Additive CNS effects are possible, including drowsiness or dizziness. Patients should report any unusual changes in moods or behaviors while taking this combination.
Armodafinil: (Major) It is not clear how armodafinil interacts with barbiturates like phenobarbital. Armodafinil is partially metabolized by CYP3A4 and combined use with CYP3A4 inducers such as phenobarbital and other barbiturates may result in decreased armodafinil efficacy. Barbiturates used for sleep could counteract the effect of armodafinil on wakefulness, and would not ordinarily be prescribed. The potential effects of combining armodafinil with anticonvulsant barbiturate medications are unclear. Many psychostimulants can reduce the seizure threshold, but it is not clear if armodafinil can affect seizure control. (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with armodafinil. Caffeine should be used cautiously with armodafinil. Intake of caffeine should be limited. Excessive intake may cause nervousness, irritability, insomnia, or other side effects.
Artemether; Lumefantrine: (Major) The barbiturates are inducers and both components of artemether; lumefantrine are substrates of the CYP3A4 isoenzyme; therefore, coadministration may lead to decreased artemether; lumefantrine concentrations. Concomitant use warrants caution due to a possible reduction in antimalarial activity.
Articaine; Epinephrine: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants. (Moderate) Coadministration of articaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue articaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
Asenapine: (Moderate) Barbiturates can cause CNS depression, and if used concomitantly with asenapine, may increase both the frequency and the intensity of adverse effects such as drowsiness, sedation, and dizziness.
Aspirin, ASA: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. High-dose, chronic administration of the combined analgesics significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Aspirin, ASA; Butalbital; Caffeine: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. High-dose, chronic administration of the combined analgesics significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy. (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Aspirin, ASA; Butalbital; Caffeine; Codeine: (Major) Concomitant use of codeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when codeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of codeine with a barbiturate can decrease codeine concentrations, resulting in less metabolism by CYP2D6 and decreased morphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of codeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4. Codeine is primarily metabolized by CYP2D6 to morphine, and by CYP3A4 to norcodeine; norcodeine does not have analgesic properties. (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. High-dose, chronic administration of the combined analgesics significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy. (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Aspirin, ASA; Caffeine; Dihydrocodeine: (Major) Concomitant use of dihydrocodeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when dihydrocodeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of dihydrocodeine with a barbiturate can decrease dihydrocodeine concentrations, resulting in less metabolism by CYP2D6 and decreased dihydromorphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of dihydrocodeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4, an isoenzyme partially responsible for the metabolism of dihydrocodeine. (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. High-dose, chronic administration of the combined analgesics significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Aspirin, ASA; Caffeine; Orphenadrine: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. High-dose, chronic administration of the combined analgesics significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Aspirin, ASA; Carisoprodol: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. High-dose, chronic administration of the combined analgesics significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Aspirin, ASA; Carisoprodol; Codeine: (Major) Concomitant use of codeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when codeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of codeine with a barbiturate can decrease codeine concentrations, resulting in less metabolism by CYP2D6 and decreased morphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of codeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4. Codeine is primarily metabolized by CYP2D6 to morphine, and by CYP3A4 to norcodeine; norcodeine does not have analgesic properties. (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. High-dose, chronic administration of the combined analgesics significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Aspirin, ASA; Citric Acid; Sodium Bicarbonate: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. High-dose, chronic administration of the combined analgesics significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy. (Minor) Antacids can delay the oral absorption of acetaminophen, but the interactions are not likely to be clinically significant as the extent of acetaminophen absorption is not appreciably affected.
Aspirin, ASA; Dipyridamole: (Major) Methylxanthines, through antagonism of adenosine and thus pharmacologic-induced coronary vasodilation, have been associated with false-negative results during dipyridamole-thallium 201 stress testing. It is recommended that methylxanthines (caffeine, caffeinated beverages and foods, theophylline, etc.) be discontinued for at least 24 hours prior to stress testing. An interaction is not expected when methylxanthines are used concomitantly with chronic dipyridamole therapy. (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. High-dose, chronic administration of the combined analgesics significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Aspirin, ASA; Omeprazole: (Major) Avoid coadministration of omeprazole with barbiturates because it can result in decreased efficacy of omeprazole. Omeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. High-dose, chronic administration of the combined analgesics significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Aspirin, ASA; Oxycodone: (Major) Concomitant use of oxycodone with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concurrent use of oxycodone with a barbiturate may decrease oxycodone plasma concentrations, decrease opioid efficacy, and potentially lead to a withdrawal syndrome in those with physical dependence to opioid agonists. Monitor for signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of increased opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; oxycodone is a CYP3A4 substrate. (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. High-dose, chronic administration of the combined analgesics significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Aspirin, ASA; Pravastatin: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. High-dose, chronic administration of the combined analgesics significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Atazanavir: (Major) Coadministration of butalbital and atazanavir may increase the metabolism of atazanavir and lead to decreased atazanavir concentrations resulting in reduction of antiretroviral efficacy and development of viral resistance. If atazanavir and butalbital are used together, the patient must be closely monitored for antiviral efficacy.
Atazanavir; Cobicistat: (Major) Coadministration of butalbital and atazanavir may increase the metabolism of atazanavir and lead to decreased atazanavir concentrations resulting in reduction of antiretroviral efficacy and development of viral resistance. If atazanavir and butalbital are used together, the patient must be closely monitored for antiviral efficacy.
Atenolol; Chlorthalidone: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Atorvastatin: (Minor) CYP3A4 inducers like the barbiturates may decrease the efficacy of atorvastatin, a CYP3A4 substrate. Monitor for potential reduced cholesterol-lowering efficacy when these drugs are co-administered.
Atorvastatin; Ezetimibe: (Minor) CYP3A4 inducers like the barbiturates may decrease the efficacy of atorvastatin, a CYP3A4 substrate. Monitor for potential reduced cholesterol-lowering efficacy when these drugs are co-administered.
Atropine; Benzoic Acid; Hyoscyamine; Methenamine; Methylene Blue; Phenyl Salicylate: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur.
Atropine; Difenoxin: (Moderate) Concurrent administration of diphenoxylate/difenoxin with barbiturates can potentiate the CNS-depressant effects of diphenoxylate/difenoxin. Use caution during coadministration.
Atropine; Diphenoxylate: (Moderate) Concurrent administration of diphenoxylate/difenoxin with barbiturates can potentiate the CNS-depressant effects of diphenoxylate/difenoxin. Use caution during coadministration.
Atropine; Hyoscyamine; Phenobarbital; Scopolamine: (Moderate) Scopolamine may cause dizziness and drowsiness. Concurrent use of scopolamine and CNS depressants can adversely increase the risk of CNS depression. (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Avanafil: (Minor) Avanafil is a substrate of and primarily metabolized by CYP3A4. It can be expected that concomitant administration of CYP3A4 enzyme-inducers will decrease plasma levels of avanafil, however, no interaction studies have been performed. CYP3A4 inducers include barbiturates.
Avatrombopag: (Major) In patients with chronic immune thrombocytopenia (ITP), increase the starting dose of avatrombopag to 40 mg PO once daily when used concomitantly with barbiturates. In patients starting barbiturates while receiving avatrombopag, monitor platelet counts and adjust the avatrombopag dose as necessary. Dosage adjustments are not required for patients with chronic liver disease. Avatrombopag is a CYP2C9 and CYP3A4 substrate, and dual moderate or strong inducers such as barbiturates decrease avatrombopag exposure, which may reduce efficacy.
Axitinib: (Major) Avoid coadministration of axitinib with butalbital if possible, due to the risk of decreased efficacy of axitinib. Selection of a concomitant medication with no or minimal CYP3A4 induction potential is recommended. Axitinib is primarily metabolized by CYP3A4. Butalbital is a moderate CYP3A4 inducer. Coadministration with a strong CYP3A4/5 inducer significantly decreased the plasma exposure of axitinib in healthy volunteers.
Azelastine: (Moderate) An enhanced CNS depressant effect may occur when azelastine, an antihistamine, is combined with CNS depressants including the barbiturates.
Azelastine; Fluticasone: (Moderate) An enhanced CNS depressant effect may occur when azelastine, an antihistamine, is combined with CNS depressants including the barbiturates. (Moderate) Coadministration may result in decreased exposure to fluticasone. Butalbital is a CYP3A4 inducer; fluticasone is a CYP3A4 substrate. Monitor for decreased response to fluticasone during concurrent use.
Azilsartan; Chlorthalidone: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Barbiturates: (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Bedaquiline: (Major) Avoid concurrent use of barbiturates with bedaquiline. Barbiturates may induce CYP3A4 metabolism resulting in decreased bedaquiline systemic exposure (AUC) and possibly reduced therapeutic effect.
Belladonna Alkaloids; Ergotamine; Phenobarbital: (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Belladonna; Opium: (Major) Concomitant use of opium with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation.
Benazepril; Hydrochlorothiazide, HCTZ: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Bendamustine: (Moderate) Bendamustine is metabolized to minimally active metabolites by CYP1A2. Concurrent administration of a CYP1A2 inducer such as the barbiturates may cause a decrease in bendamustine plasma concentrations and a potential decrease in cytotoxicity. The parent compound of Bendamustine is believed to be primarily responsible for the cytotoxicity against cancers. Caution should be exercised when coadministering bendamustine with a CYP1A2 inducer, or consider an alternative agent.
Bendroflumethiazide; Nadolol: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Benzhydrocodone; Acetaminophen: (Major) Concomitant use of benzhydrocodone with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concurrent use of benzhydrocodone with a barbiturate may decrease benzhydrocodone plasma concentrations, decrease opioid efficacy, and potentially lead to a withdrawal syndrome in those with physical dependence to opioid agonists. Monitor for signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of increased opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; benzhydrocodone is a CYP3A4 substrate.
Benzodiazepines: (Minor) Patients taking benzodiazepines for insomnia should not use caffeine-containing products prior to going to bed as these products may antagonize the sedative effects of the benzodiazepine.
Benzoic Acid; Hyoscyamine; Methenamine; Methylene Blue; Phenyl Salicylate: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur.
Benzphetamine: (Moderate) Avoid excessive caffeine intake during use of benzphetamine. Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants. Excessive caffeine ingestion (via medicines, foods like chocolate, dietary supplements, or beverages including coffee, green tea, other teas, colas) may contribute to side effects like nervousness, irritability, nausea, insomnia, or tremor. Patients should avoid medications and dietary supplements which contain high amounts of caffeine.
Benztropine: (Moderate) CNS depressants, such as anxiolytics, sedatives, and hypnotics, can increase the sedative effects of benztropine.
Beta-agonists: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Bicalutamide: (Moderate) Bicalutamide is metabolized by CYP3A4. Barbiturates induce CYP3A4 activity and will decrease the plasma concentrations of bicalutamide.
Bismuth Subcitrate Potassium; Metronidazole; Tetracycline: (Minor) Barbiturates may decrease the half-life and plasma concentrations of metronidazole. The clinical significance of this effect is uncertain.
Bismuth Subsalicylate: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. Although salicylates are rarely associated with nephrotoxicity, high-dose, chronic administration of salicylates combined other analgesics, including acetaminophen, significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Additive hepatic toxicity may occur, especially in combined overdose situations. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Bismuth Subsalicylate; Metronidazole; Tetracycline: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. Although salicylates are rarely associated with nephrotoxicity, high-dose, chronic administration of salicylates combined other analgesics, including acetaminophen, significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Additive hepatic toxicity may occur, especially in combined overdose situations. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy. (Minor) Barbiturates may decrease the half-life and plasma concentrations of metronidazole. The clinical significance of this effect is uncertain.
Bisoprolol; Hydrochlorothiazide, HCTZ: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Boceprevir: (Moderate) Close clinical monitoring is advised when administering acetaminophen with boceprevir due to an increased potential for acetaminophen-related adverse events. If acetaminophen dose adjustments are made, re-adjust the dose upon completion of boceprevir treatment. Although this interaction has not been studied, predictions about the interaction can be made based on the metabolic pathway of acetaminophen. Acetaminophen is partially metabolized by the hepatic isoenzyme CYP3A4; boceprevir inhibits this isoenzyme. Coadministration may result in elevated acetaminophen plasma concentrations.
Bortezomib: (Moderate) Because bortezomib undergoes significant metabolism by the cytochrome P450 system, induction of CYP450 enzymes by the barbiturates may increase the clearance and metabolism of this drug and may result in decreased therapeutic effects.
Brexpiprazole: (Major) Because brexpiprazole is partially metabolized by CYP3A4, the manufacturer recommends that the brexpiprazole dose be doubled over 1 to 2 weeks when strong CYP3A4 inducers, such as barbiturates and primidone, are added to brexpiprazole therapy. If these agents are used in combination, the patient should be carefully monitored for a decrease in brexpiprazole efficacy. When the CYP3A4 inducer is withdrawn from the combination therapy, the brexpiprazole dose should be reduced over 1 to 2 weeks to the original level.
Brigatinib: (Major) Avoid coadministration of brigatinib with butalbital due to decreased plasma exposure to brigatinib which may result in decreased efficacy. If concomitant use is unavoidable, after 7 days of concomitant treatment with butalbital, increase the dose of brigatinib as tolerated in 30 mg increments to a maximum of twice the original brigatinib dose. After discontinuation of butalbital, resume the brigatinib dose that was tolerated prior to initiation of butalbital. Brigatinib is a CYP3A4 substrate and butalbital is a moderate CYP3A4 inducer. Coadministration with a moderate CYP3A inducer is predicted to decrease the AUC of brigatinib by approximately 50%.
Brimonidine: (Moderate) Based on the sedative effects of brimonidine in individual patients, brimonidine administration has potential to enhance the CNS depressants effects of the anxiolytics, sedatives, and hypnotics including barbiturates.
Brimonidine; Brinzolamide: (Moderate) Based on the sedative effects of brimonidine in individual patients, brimonidine administration has potential to enhance the CNS depressants effects of the anxiolytics, sedatives, and hypnotics including barbiturates.
Brimonidine; Timolol: (Moderate) Based on the sedative effects of brimonidine in individual patients, brimonidine administration has potential to enhance the CNS depressants effects of the anxiolytics, sedatives, and hypnotics including barbiturates.
Brivaracetam: (Minor) Plasma concentrations of brivaracetam may decrease during co-administration with barbiturates. A 19% decrease in the plasma concentration of brivaracetam was observed during co-administration with phenobarbital; however, no dose adjustment is recommended for brivaracetam during concomitant therapy.
Bromocriptine: (Moderate) Caution and close monitoring are advised if bromocriptine and butalbital are used together. Concurrent use may decrease the plasma concentrations of bromocriptine resulting in loss of efficacy. Bromocriptine is extensively metabolized by the liver via CYP3A4; butalbital is a moderate inducer of CYP3A4.
Brompheniramine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as brompheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities.
Brompheniramine; Carbetapentane; Phenylephrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as brompheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor. (Moderate) Drowsiness has been reported during administration of carbetapentane. An enhanced CNS depressant effect may occur when carbetapentane is combined with other CNS depressants including barbiturates.
Brompheniramine; Dextromethorphan; Guaifenesin: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as brompheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities.
Brompheniramine; Guaifenesin; Hydrocodone: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate. (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as brompheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities.
Brompheniramine; Hydrocodone; Pseudoephedrine: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate. (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as brompheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Brompheniramine; Pseudoephedrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as brompheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Budesonide: (Moderate) Coadministration may result in decreased exposure to budesonide. Butalbital is a CYP3A4 inducer; budesonide is a CYP3A4 substrate. Monitor for decreased response to budesonide during concurrent use.
Budesonide; Formoterol: (Moderate) Coadministration may result in decreased exposure to budesonide. Butalbital is a CYP3A4 inducer; budesonide is a CYP3A4 substrate. Monitor for decreased response to budesonide during concurrent use. (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Bupivacaine Liposomal: (Moderate) Coadministration of bupivacaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue bupivacaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen. (Minor) Bupivacaine is metabolized by CYP3A4. Barbiturates induce these isoenzymes and if given concurrently with bupivacaine may decrease the efficacy of bupivacaine.
Bupivacaine: (Moderate) Coadministration of bupivacaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue bupivacaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen. (Minor) Bupivacaine is metabolized by CYP3A4. Barbiturates induce these isoenzymes and if given concurrently with bupivacaine may decrease the efficacy of bupivacaine.
Bupivacaine; Lidocaine: (Moderate) Coadministration of bupivacaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue bupivacaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen. (Moderate) Coadministration of lidocaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue lidocaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen. (Minor) Bupivacaine is metabolized by CYP3A4. Barbiturates induce these isoenzymes and if given concurrently with bupivacaine may decrease the efficacy of bupivacaine.
Buprenorphine: (Moderate) Close monitoring of the patient is recommended if a CYP3A4 inducer is used with buprenorphine. Inducers of CYP3A4 such as phenobarbital may induce the hepatic metabolism of buprenorphine, which may lead to opiate withdrawal or inadequate pain control. It is likely that all barbiturates exert the same effect as phenobarbital. This interaction is most significant if the enzyme-inducing agent is added after buprenorphine therapy has begun. Buprenorphine doses may need to be increased if any of these agents are added. Conversely, buprenorphine doses may need to be decreased if these drugs are discontinued. Additive CNS depression may be the more important issue initially when barbiturates are given with buprenorphine; the induction of buprenorphine metabolism may take several days. Prior to concurrent use of buprenorphine in patients taking a CNS depressant, assess the level of tolerance to CNS depression that has developed, the duration of use, and the patient’s overall response to treatment. Consider the patient’s use of alcohol or illicit drugs. A dose reduction of one or both drugs may be warranted. It is recommended that the injectable buprenorphine dose be halved for patients who receive other drugs with CNS depressant effects; for the buprenorphine transdermal patch, start with the 5 mcg/hour patch. Monitor patients for sedation or respiratory depression.
Buprenorphine; Naloxone: (Moderate) Close monitoring of the patient is recommended if a CYP3A4 inducer is used with buprenorphine. Inducers of CYP3A4 such as phenobarbital may induce the hepatic metabolism of buprenorphine, which may lead to opiate withdrawal or inadequate pain control. It is likely that all barbiturates exert the same effect as phenobarbital. This interaction is most significant if the enzyme-inducing agent is added after buprenorphine therapy has begun. Buprenorphine doses may need to be increased if any of these agents are added. Conversely, buprenorphine doses may need to be decreased if these drugs are discontinued. Additive CNS depression may be the more important issue initially when barbiturates are given with buprenorphine; the induction of buprenorphine metabolism may take several days. Prior to concurrent use of buprenorphine in patients taking a CNS depressant, assess the level of tolerance to CNS depression that has developed, the duration of use, and the patient’s overall response to treatment. Consider the patient’s use of alcohol or illicit drugs. A dose reduction of one or both drugs may be warranted. It is recommended that the injectable buprenorphine dose be halved for patients who receive other drugs with CNS depressant effects; for the buprenorphine transdermal patch, start with the 5 mcg/hour patch. Monitor patients for sedation or respiratory depression.
Bupropion: (Moderate) Bupropion is associated with a dose-related risk of seizures. Excessive use of psychostimulants, including caffeine, is associated with an increased seizure risk and may increase this risk during the concurrent use of bupropion. Carefully consider a patient’s caffeine intake from all sources, including medicines. Monitor for irritability, tremor, increased blood pressure, insomnia and seizures. Many non-prescription medicines and weight loss aids may contain caffeine and patients should read labels carefully. Examples of foods and beverages containing caffeine include coffee, teas, colas, energy drinks, chocolate, and some herbal or dietary supplements. Patients should be advised to limit excessive caffeine intake during bupropion therapy. (Moderate) Bupropion may interact with drugs that induce hepatic microsomal isoenzyme function via CYP2B6 such as the barbiturates. While not systematically studied, these drugs may induce the metabolism of bupropion and may decrease bupropion exposure. If bupropion is used concomitantly with a CYP inducer, it may be necessary to increase the dose of bupropion, but the maximum recommended dose should not be exceeded. Advise patients that until they are reasonably certain that the combination does not adversely affect their performance, they should refrain from driving an automobile or operating complex, hazardous machinery.
Bupropion; Naltrexone: (Moderate) Bupropion is associated with a dose-related risk of seizures. Excessive use of psychostimulants, including caffeine, is associated with an increased seizure risk and may increase this risk during the concurrent use of bupropion. Carefully consider a patient’s caffeine intake from all sources, including medicines. Monitor for irritability, tremor, increased blood pressure, insomnia and seizures. Many non-prescription medicines and weight loss aids may contain caffeine and patients should read labels carefully. Examples of foods and beverages containing caffeine include coffee, teas, colas, energy drinks, chocolate, and some herbal or dietary supplements. Patients should be advised to limit excessive caffeine intake during bupropion therapy. (Moderate) Bupropion may interact with drugs that induce hepatic microsomal isoenzyme function via CYP2B6 such as the barbiturates. While not systematically studied, these drugs may induce the metabolism of bupropion and may decrease bupropion exposure. If bupropion is used concomitantly with a CYP inducer, it may be necessary to increase the dose of bupropion, but the maximum recommended dose should not be exceeded. Advise patients that until they are reasonably certain that the combination does not adversely affect their performance, they should refrain from driving an automobile or operating complex, hazardous machinery.
Buspirone: (Moderate) Monitor for reduced anxiolytic effect of buspirone. Potent inducers of CYP3A4, such as the barbiturates, may increase the rate of buspirone metabolism. If a patient has been titrated to a stable dosage on buspirone, a dose adjustment of buspirone may be necessary to maintain anxiolytic effect. There is also a risk of additive CNS depression (drowsiness) when buspirone is given concomitantly with barbiturates. In a study in healthy volunteers, co-administration of buspirone with a potent CYP3A4 inducer decreased the plasma concentrations (83.7% decrease in Cmax; 89.6% decrease in AUC) and pharmacodynamic effects of buspirone.
Busulfan: (Moderate) Use busulfan and acetaminophen together with caution; concomitant use may result in increased busulfan levels and increased busulfan toxicity. Separating the administration of these drugs may mitigate this interaction; avoid giving acetaminophen within 72 hours prior to or concurrently with busulfan. Busulfan is metabolized in the liver through conjugation with glutathione; acetaminophen decreases glutathione levels in the blood and tissues and may reduce the clearance of busulfan.
Butabarbital: (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Butorphanol: (Moderate) Concomitant use of butorphanol with other CNS depressants, such as barbiturates, can potentiate the effects of butorphanol on respiratory depression, CNS depression, and sedation.
Caffeine: (Moderate) Certain foods that contain high amounts of caffeine or theobromine should be limited during the therapeutic use of caffeine in order to limit additive methylxanthine effects. While taking Caffeine-containing medicines, limit the use of foods, beverages (examples: coffee, tea, colas), herbs (examples: guarana, green tea) and other products that contain additional caffeine, such as chocolate and some non-prescription medications or dietary supplements for headache, insomnia, or weight loss. Too much Caffeine can cause effects like nausea, nervousness, or sleeplessness. Some drug products for adults that contain caffeine have about as much caffeine as a cup of coffee. (Minor) The hypnotic effects of barbiturates can be reduced by caffeine administration.
Calcifediol: (Moderate) Dose adjustment of calcifediol may be necessary during coadministration with barbiturates. Additionally, serum 25-hydroxyvitamin D, intact PTH, and calcium concentrations should be closely monitored if a patient initiates or discontinues therapy with barbiturates. Barbiturates stimulate microsomal hydroxylation and reduce the half-life of calcifediol. In rare cases, this has caused anticonvulsant-induced rickets and osteomalacia.
Calcitriol: (Moderate) Barbiturates can decrease the activity of vitamin D by increasing its metabolism. In rare cases, this has caused anticonvulsant-induced rickets and osteomalacia. Vitamin D supplementation may be required in patients with inadequate dietary intake of vitamin D who are receiving chronic treatment with barbiturates.
Candesartan; Hydrochlorothiazide, HCTZ: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Cannabidiol: (Moderate) Consider a dose adjustment of caffeine when coadministered with cannabidiol. Coadministration may alter plasma concentrations of caffeine resulting in an increased risk of adverse reactions and/or decreased efficacy. Caffeine is a sensitive CYP1A2 substrate. In vitro data predicts inhibition or induction of CYP1A2 by cannabidiol potentially resulting in clinically significant interactions. (Moderate) Monitor for excessive sedation and somnolence during coadministration of cannabidiol and butalbital. CNS depressants can potentiate the effects of cannabidiol.
Captopril; Hydrochlorothiazide, HCTZ: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Carbamazepine: (Moderate) Barbiturates can accelerate hepatic metabolism of carbamazepine due to induction of hepatic microsomal enzyme activity. Carbamazepine serum concentrations should be monitored closely if a barbiturate is added or discontinued during therapy. (Minor) Carbamazepine may induce caffeine metabolism via induction of the hepatic CYP1A2 isoenzyme. (Minor) Carbamazepine may potentially accelerate the hepatic metabolism of acetaminophen. In addition, due to enzyme induction, carbamazepine may increase the risk for acetaminophen-induced hepatotoxicity via generation of a greater percentage of acetaminophen’s hepatotoxic metabolite, NAPQI. Clinicians should be alert to decreased effect of acetaminophen. Dosage adjustments may be necessary, and closer monitoring of clinical and/or adverse effects is warranted.
Carbetapentane; Chlorpheniramine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) Drowsiness has been reported during administration of carbetapentane. An enhanced CNS depressant effect may occur when carbetapentane is combined with other CNS depressants including barbiturates.
Carbetapentane; Chlorpheniramine; Phenylephrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor. (Moderate) Drowsiness has been reported during administration of carbetapentane. An enhanced CNS depressant effect may occur when carbetapentane is combined with other CNS depressants including barbiturates.
Carbetapentane; Diphenhydramine; Phenylephrine: (Major) Because diphenhydramine can cause pronounced sedation, an enhanced CNS depressant effect may occur when it is combined with other CNS depressants including anxiolytics, sedatives, and hypnotics, such as barbiturates. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor. (Moderate) Drowsiness has been reported during administration of carbetapentane. An enhanced CNS depressant effect may occur when carbetapentane is combined with other CNS depressants including barbiturates.
Carbetapentane; Guaifenesin: (Moderate) Drowsiness has been reported during administration of carbetapentane. An enhanced CNS depressant effect may occur when carbetapentane is combined with other CNS depressants including barbiturates.
Carbetapentane; Guaifenesin; Phenylephrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor. (Moderate) Drowsiness has been reported during administration of carbetapentane. An enhanced CNS depressant effect may occur when carbetapentane is combined with other CNS depressants including barbiturates.
Carbetapentane; Phenylephrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor. (Moderate) Drowsiness has been reported during administration of carbetapentane. An enhanced CNS depressant effect may occur when carbetapentane is combined with other CNS depressants including barbiturates.
Carbetapentane; Phenylephrine; Pyrilamine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor. (Moderate) Drowsiness has been reported during administration of carbetapentane. An enhanced CNS depressant effect may occur when carbetapentane is combined with other CNS depressants including barbiturates.
Carbetapentane; Pseudoephedrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor. (Moderate) Drowsiness has been reported during administration of carbetapentane. An enhanced CNS depressant effect may occur when carbetapentane is combined with other CNS depressants including barbiturates.
Carbetapentane; Pyrilamine: (Moderate) Drowsiness has been reported during administration of carbetapentane. An enhanced CNS depressant effect may occur when carbetapentane is combined with other CNS depressants including barbiturates.
Carbidopa; Levodopa; Entacapone: (Moderate) COMT inhibitors, like entacapone or tolcapone, should be given cautiously with other agents that cause CNS depression due to the possibility of additive sedation. Agents that may cause additive sedation when given concurrently with tolcapone include the barbiturates. The risk for adverse effects may increase, and patients should use caution in driving or other hazardous tasks until the effects of the drugs are known.
Carbinoxamine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as carbinoxamine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities.
Carbinoxamine; Dextromethorphan; Pseudoephedrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as carbinoxamine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Carbinoxamine; Hydrocodone; Phenylephrine: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate. (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as carbinoxamine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Carbinoxamine; Hydrocodone; Pseudoephedrine: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate. (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as carbinoxamine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Carbinoxamine; Phenylephrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as carbinoxamine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Carbinoxamine; Pseudoephedrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as carbinoxamine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Cardiac glycosides: (Moderate) Hepatic enzyme inducing drugs, such as barbiturates, can accelerate the metabolism of digoxin, decreasing its serum concentrations. It is recommended that digoxin concentrations be monitored if used with barbiturates.
Cariprazine: (Major) Cariprazine and its active metabolites are extensively metabolized by CYP3A4. Concurrent use of cariprazine with CYP3A4 inducers, such as primidone or barbiturates, has not been evaluated and is not recommended because the net effect on active drug and metabolites is unclear. In addition, due to the CNS effects of cariprazine, caution should be used when cariprazine is given in combination with other centrally-acting medications including benzodiazepines and other anxiolytics, sedatives, and hypnotics.
Cetirizine: (Moderate) Concurrent use of cetirizine/levocetirizine with barbiturates should generally be avoided. Coadministration may increase the risk of CNS depressant-related side effects. If concurrent use is necessary, monitor for excessive sedation and somnolence.
Cetirizine; Pseudoephedrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor. (Moderate) Concurrent use of cetirizine/levocetirizine with barbiturates should generally be avoided. Coadministration may increase the risk of CNS depressant-related side effects. If concurrent use is necessary, monitor for excessive sedation and somnolence.
Cevimeline: (Moderate) Inducers of cytochrome P450 3A4 and/or CYP 2D6, such as the barbiturates, may cause a reduction in cevimeline plasma concentrations.
Charcoal: (Minor) Activated charcoal binds many drugs within the gut. Administering charcoal dietary supplements at the same time as a routine acetaminophen dosage would be expected to interfere with the analgesic and antipyretic efficacy of acetaminophen. Charcoal is mostly used in the setting of acetaminophen overdose; however, patients should never try to treat an acetaminophen overdose with charcoal dietary supplements. Advise patients to get immediate medical attention for an acetaminophen overdose.
Chlophedianol; Dexchlorpheniramine; Pseudoephedrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as dexchlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Chlophedianol; Guaifenesin; Phenylephrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Chlorambucil: (Minor) Barbiturates appear to increase the hepatic activation of chlorambucil to its active metabolite than to inactive metabolite. Clinicians should be alert for a potential increase in chlorambucil related activity and/or toxicity.
Chloramphenicol: (Moderate) Chloramphenicol inhibits the cytochrome P-450 enzyme system and can affect the hepatic metabolism of phenobarbital. Phenobarbital levels rise modestly. It is also possible that plasma concentrations of chloramphenicol can be reduced by concomitant use of barbiturates, agents that are known to stimulate hepatic microsomal enzymes responsible for chloramphenicol metabolism.
Chlordiazepoxide: (Moderate) Additive CNS and/or respiratory depression may occur. Additionally, barbiturates may increase the metabolism of chlordiazepoxide. Chlordiazepoxide is a CYP3A4 substrate. Barbiturates are CYP3A4 inducers.
Chlordiazepoxide; Clidinium: (Moderate) Additive CNS and/or respiratory depression may occur. Additionally, barbiturates may increase the metabolism of chlordiazepoxide. Chlordiazepoxide is a CYP3A4 substrate. Barbiturates are CYP3A4 inducers.
Chloroprocaine: (Moderate) Coadministration of chloroprocaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue chloroprocaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
Chlorothiazide: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Chlorpheniramine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities.
Chlorpheniramine; Codeine: (Major) Concomitant use of codeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when codeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of codeine with a barbiturate can decrease codeine concentrations, resulting in less metabolism by CYP2D6 and decreased morphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of codeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4. Codeine is primarily metabolized by CYP2D6 to morphine, and by CYP3A4 to norcodeine; norcodeine does not have analgesic properties. (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities.
Chlorpheniramine; Dextromethorphan: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities.
Chlorpheniramine; Dextromethorphan; Phenylephrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Chlorpheniramine; Dihydrocodeine; Phenylephrine: (Major) Concomitant use of dihydrocodeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when dihydrocodeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of dihydrocodeine with a barbiturate can decrease dihydrocodeine concentrations, resulting in less metabolism by CYP2D6 and decreased dihydromorphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of dihydrocodeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4, an isoenzyme partially responsible for the metabolism of dihydrocodeine. (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Chlorpheniramine; Dihydrocodeine; Pseudoephedrine: (Major) Concomitant use of dihydrocodeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when dihydrocodeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of dihydrocodeine with a barbiturate can decrease dihydrocodeine concentrations, resulting in less metabolism by CYP2D6 and decreased dihydromorphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of dihydrocodeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4, an isoenzyme partially responsible for the metabolism of dihydrocodeine. (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Chlorpheniramine; Guaifenesin; Hydrocodone; Pseudoephedrine: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate. (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Chlorpheniramine; Hydrocodone: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate. (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities.
Chlorpheniramine; Hydrocodone; Phenylephrine: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate. (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Chlorpheniramine; Hydrocodone; Pseudoephedrine: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate. (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Chlorpheniramine; Phenylephrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Chlorpheniramine; Pseudoephedrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as chlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Chlorthalidone: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Chlorthalidone; Clonidine: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Cholestyramine: (Moderate) Cholestyramine has been shown to decrease the absorption of acetaminophen by roughly 60%. Experts have recommended that cholestyramine not be given within 1 hour of acetaminophen if analgesic or antipyretic effect is to be achieved.
Choline Salicylate; Magnesium Salicylate: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. Although salicylates are rarely associated with nephrotoxicity, high-dose, chronic administration of salicylates combined other analgesics, including acetaminophen, significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Additive hepatic toxicity may occur, especially in combined overdose situations. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Cimetidine: (Minor) Inhibitors of CYP1A2, such as cimetidine, may inhibit the hepatic oxidative metabolism of caffeine. In patients who complain of caffeine-related side effects caffeine dosage or intake may need to be reduced.
Cinacalcet: (Moderate) Coadministration of cinacalcet with a CYP3A4 enzyme inducer, such as a barbiturate, may result in a decreased effect of cinacalcet.
Ciprofloxacin: (Moderate) Reduction or limitation of the caffeine dosage in medications and limitation of caffeine in beverages and food may be necessary during concurrent ciprofloxacin therapy. Ciprofloxacin can decrease the clearance of caffeine. Caffeine toxicity may occur and can manifest as nausea, vomiting, anxiety, tachycardia, or seizures. Ciprofloxacin is a CYP1A2 inhibitor and caffeine is a CYP1A2 substrate.
Citalopram: (Moderate) Citalopram is metabolized by CYP2C19 and CYP3A4. Barbiturates can induce the metabolism of various CYP 450 isoenzymes, including those involved in citalopram metabolism. Although no clinical data are available to support a clinically significant interaction, citalopram may need to be administered in higher doses in patients chronically taking barbiturates.
Clemastine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as clemastine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities.
Clindamycin: (Moderate) Concomitant use of clindamycin and butalbital may increase clindamycin clearance and result in loss of efficacy of clindamycin. Clindamycin is a CYP3A4 substrate; butalbital is a moderate inducer of CYP3A4. Caution and close monitoring are advised if these drugs are used together.
Clobazam: (Moderate) Concomitant of clobazam with other CNS-depressant drugs including barbiturates can potentiate the CNS effects (i.e., increased sedation or respiratory depression) of either agent. The primary metabolic pathway of clobazam is CYP3A4, and to a lesser extent, CYP2C19 and CYP2B6. Metabolism of N-desmethylclobazam occurs primarily through CYP2C19. Results of a population pharmacokinetic analysis showed that concurrent use of phenobarbital, a CYP3A4 and CYP2C9 inducer, did not significantly alter the kinetics of clobazam or its active metabolite N-desmethylclobazam at steady-state. It should be noted that because clobazam is metabolized by multiple enzyme systems, induction of one pathway may not appreciably increase its clearance.
Clonazepam: (Moderate) Monitoring of clonazepam concentrations or dosage adjustment may be necessary if used concurrently with barbiturates due to decreased clonazepam concentrations. Clonazepam concentration decreases of approximately 38% have been reported when clonazepam is used with strong CYP3A4 inducers. Clonazepam is a CYP3A4 substrate. Barbiturates are strong CYP3A4 inducers. Additive CNS and/or respiratory depression may also occur.
Clorazepate: (Moderate) Additive CNS and/or respiratory depression may occur. Additionally, barbiturates may increase the metabolism of N-desmethyldiazepam, the active metabolite of clorazepate. N-desmethyldiazepam is a CYP3A4 and CYP2C19 substrate. Barbiturates are CYP3A4 and CYP2C19 inducers.
Clozapine: (Major) Caffeine may inhibit clozapine metabolism via CYP1A2. Clozapine clearance has been decreased by roughly 14 percent during coadministration of caffeine, and a documented increase in clozapine serum concentrations has occurred in selected patients. In addition, a single case report associates the appearance of psychiatric symptoms with caffeine ingestion in one patient taking clozapine. Until more data are available, caffeine consumption should be minimized during clozapine treatment. (Moderate) Patients on certain anticonvulsant therapies should receive clozapine with caution. Clozapine may interact with anticonvulsants in several ways; concurrent use of clozapine in patients on antiepileptic medications is not recommended in seizures that are not well controlled. Clozapine lowers the seizure threshold in a dose-dependent manner and thus may induce seizures; dosage adjustments of clozapine should be cautious. CYP1A2, CYP3A4, and CYP2D6 isoenzymes metabolize clozapine; anticonvulsant drugs known to induce one or more of these isoenzymes include barbiturates. Clinicians should monitor for reduced clozapine effectiveness during concurrent use of anticonvulsants that are weak to moderate CYP inducers. Additive sedation may be noted initially with concurrent clozapine and barbiturate use; enzyme induction by barbiturates takes several days to become clinically apparent.
Cobimetinib: (Major) Avoid the concurrent use of cobimetinib with butalbital due to decreased cobimetinib efficacy. Cobimetinib is a CYP3A substrate in vitro, and butalbital is a moderate inducer of CYP3A. Based on simulations, cobimetinib exposure would decrease by 73% when coadministered with a moderate CYP3A inducer.
Codeine: (Major) Concomitant use of codeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when codeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of codeine with a barbiturate can decrease codeine concentrations, resulting in less metabolism by CYP2D6 and decreased morphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of codeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4. Codeine is primarily metabolized by CYP2D6 to morphine, and by CYP3A4 to norcodeine; norcodeine does not have analgesic properties.
Codeine; Guaifenesin: (Major) Concomitant use of codeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when codeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of codeine with a barbiturate can decrease codeine concentrations, resulting in less metabolism by CYP2D6 and decreased morphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of codeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4. Codeine is primarily metabolized by CYP2D6 to morphine, and by CYP3A4 to norcodeine; norcodeine does not have analgesic properties.
Codeine; Phenylephrine; Promethazine: (Major) Concomitant use of codeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when codeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of codeine with a barbiturate can decrease codeine concentrations, resulting in less metabolism by CYP2D6 and decreased morphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of codeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4. Codeine is primarily metabolized by CYP2D6 to morphine, and by CYP3A4 to norcodeine; norcodeine does not have analgesic properties. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Codeine; Promethazine: (Major) Concomitant use of codeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when codeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of codeine with a barbiturate can decrease codeine concentrations, resulting in less metabolism by CYP2D6 and decreased morphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of codeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4. Codeine is primarily metabolized by CYP2D6 to morphine, and by CYP3A4 to norcodeine; norcodeine does not have analgesic properties.
COMT inhibitors: (Moderate) COMT inhibitors, like entacapone or tolcapone, should be given cautiously with other agents that cause CNS depression due to the possibility of additive sedation. Agents that may cause additive sedation when given concurrently with tolcapone include the barbiturates. The risk for adverse effects may increase, and patients should use caution in driving or other hazardous tasks until the effects of the drugs are known.
Conjugated Estrogens: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Conjugated Estrogens; Bazedoxifene: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Conjugated Estrogens; Medroxyprogesterone: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Cyclophosphamide: (Minor) Use caution if cyclophosphamide is used concomitantly with barbiturates, and monitor for a possible increase in cyclophosphamide-related adverse events. The clinical significance of this interaction is unknown. Cyclophosphamide is a prodrug that is hydroxylated and activated primarily by CYP2B6; the contribution of CYP3A4 to the activation of cyclophosphamide is variable. N-dechloroethylation to therapeutically inactive but neurotoxic metabolites occurs primarily via CYP3A4. Additional isoenzymes involved in the activation of cyclophosphamide include CYP2C9 and 2C19. The active metabolites, 4-hydroxycyclophosphamide and aldophosphamide, are inactivated by aldehyde dehydrogenase-mediated oxidation. Barbiturates are CYP3A4 inducers, as well as inducers of CYP2C9 and 2C19. It is not yet clear what effects CYP450 inducers have on the activation and/or toxicity of cyclophosphamide; the production of active or neurotoxic metabolites may be increased.
Cyclosporine: (Major) Phenobarbital may induce cyclosporine metabolism, thereby increasing the clearance of cyclosporine. It is likely that other barbiturates would interact similarly with cyclosporine; however no supportive data are available. If phenobarbital is added to an existing cyclosporine regimen, monitor cyclosporine concentrations closely to avoid loss of clinical efficacy until a new steady-state concentration is achieved. Conversely, if phenobarbital is discontinued, cyclosporine concentrations could increase.
Cyproheptadine: (Moderate) Additive CNS depression may occur if barbiturates are used concomitantly with cyproheptadine.
Dapsone: (Moderate) Coadministration of dapsone with acetaminophen may increase the risk of developing methemoglobinemia. Advise patients to discontinue treatment and seek immediate medical attention with any signs or symptoms of methemoglobinemia.
Darifenacin: (Minor) Barbiturates (e.g., phenobarbital or primidone) may induce the CYP3A4 metabolism of darifenacin. The dosage requirements of darifenacin may be increased in patients receiving concurrent enzyme inducers. (Minor) Consuming > 400 mg/day caffeine has been associated with the development of urinary incontinence. Caffeine may aggravate bladder symptoms, increase urination, and counteract the effectiveness of darifenacin to some degree. Patients may wish to limit their intake of caffeinated drugs, dietary supplements (e.g., guarana), or beverages (e.g., green tea, other teas, coffee, colas).
Darunavir: (Major) Coadministration of butalbital and darunavir may increase the metabolism of darunavir and lead to decreased darunavir concentrations resulting in reduction of antiretroviral efficacy and development of viral resistance. If darunavir and butalbital are used together, the patient must be closely monitored for antiviral efficacy.
Darunavir; Cobicistat: (Major) Coadministration of butalbital and darunavir may increase the metabolism of darunavir and lead to decreased darunavir concentrations resulting in reduction of antiretroviral efficacy and development of viral resistance. If darunavir and butalbital are used together, the patient must be closely monitored for antiviral efficacy.
Darunavir; Cobicistat; Emtricitabine; Tenofovir alafenamide: (Major) Coadministration of butalbital and darunavir may increase the metabolism of darunavir and lead to decreased darunavir concentrations resulting in reduction of antiretroviral efficacy and development of viral resistance. If darunavir and butalbital are used together, the patient must be closely monitored for antiviral efficacy.
Dasabuvir; Ombitasvir; Paritaprevir; Ritonavir: (Major) Concurrent use of ritonavir with phenobarbital or other barbiturates should be done cautiously. Increased doses of anticonvulsants may be required due metabolism induction by ritonavir. However, since these anticonvulsants are hepatic enzyme inducing drugs, increased metabolism of protease inhibitors may occur, leading to decreased antiretroviral efficacy. Close monitoring of drug concentrations and/or therapeutic and adverse effects is required. (Moderate) Concurrent administration of acetaminophen with ritonavir may result in elevated acetaminophen plasma concentrations and subsequent adverse events. Acetaminophen is metabolized by the hepatic isoenzyme CYP3A4; ritonavir is an inhibitor of this enzyme. Caution and close monitoring are advised if these drugs are administered together.
Deflazacort: (Major) Avoid concomitant use of deflazacort and butalbital. Concurrent use may significantly decrease concentrations of 21-desDFZ, the active metabolite of deflazacort, resulting in loss of efficacy. Deflazacort is a CYP3A4 substrate; butalbital is a moderate inducer of CYP3A4. Administration of deflazacort with multiple doses of rifampin (a strong CYP3A4 inducer) resulted in geometric mean exposures that were approximately 95% lower compared to administration alone.
Delavirdine: (Major) Barbiturates may increase the metabolism of delavirdine, lead to substantial reductions in delavirdine concentrations and efficacy. The manufacturer recommends that delavirdine not be given with barbiturates when used as anticonvulsants due to the potential for subtherapeutic antiretroviral activity and the subsequent possibility for the development of resistant mutations of HIV. In addition, delavirdine may inhibit the metabolism of the barbiturates. If used concomitantly, the patient should be observed for changes in the clinical efficacy and concentrations of the antiretroviral and anticonvulsant regimens.
Desloratadine; Pseudoephedrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Deutetrabenazine: (Moderate) Advise patients that concurrent use of deutetrabenazine and drugs that can cause CNS depression, such as barbiturates, may have additive effects and worsen drowsiness or sedation.
Dexamethasone: (Moderate) Coadministration may result in decreased exposure to dexamethasone. Butalbital is a CYP3A4 inducer; dexamethasone is a CYP3A4 substrate. Monitor for decreased response to dexamethasone during concurrent use.
Dexchlorpheniramine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as dexchlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities.
Dexchlorpheniramine; Dextromethorphan; Pseudoephedrine: (Moderate) Additive CNS depression may occur if barbiturates are co-used with sedating antihistamines, such as dexchlorpheniramine. Monitor for additive CNS and respiratory effects, and warn about the potential effects to driving and other activities. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Dexlansoprazole: (Major) Avoid coadministration of dexlansoprazole with barbiturates because it may result in decreased efficacy of dexlansoprazole. Dexlansoprazole is metabolized by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19.
Dexmedetomidine: (Moderate) Co-administration of dexmedetomidine with barbiturates is likely to lead to an enhancement of CNS depression.
Dexmethylphenidate: (Moderate) Caffeine is a CNS stimulant and such actions are expected to be additive when coadministered with psychostimulants such as dexmethylphenidate. Avoid excessive caffeine intake during use of dexmethylphenidate. Excessive caffeine ingestion (via medicines, foods like chocolate, dietary supplements, or beverages including coffee, green tea, other teas, colas) may contribute to side effects like nervousness, irritability, nausea, insomnia, tachycardia, or tremor. Patients should avoid medications and dietary supplements which contain high amounts of caffeine.
Dextroamphetamine: (Moderate) Avoid excessive caffeine intake during use of the amphetamine salts. Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants. Excessive caffeine ingestion (via medicines, foods like chocolate, dietary supplements, or beverages including coffee, green tea, other teas, colas) may contribute to side effects like nervousness, irritability, nausea, insomnia, or tremor. Patients should avoid medications and dietary supplements which contain high amounts of caffeine.
Dextromethorphan; Diphenhydramine; Phenylephrine: (Major) Because diphenhydramine can cause pronounced sedation, an enhanced CNS depressant effect may occur when it is combined with other CNS depressants including anxiolytics, sedatives, and hypnotics, such as barbiturates. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Dextromethorphan; Guaifenesin; Phenylephrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Dextromethorphan; Guaifenesin; Pseudoephedrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Dextromethorphan; Quinidine: (Major) Quinidine is eliminated primarily via hepatic metabolism, primarily by the CYP3A4 isoenzyme. Administration of other hepatic enzyme inducers, such as barbiturates, can accelerate quinidine elimination and decrease its serum concentrations. Phenobarbital may decrease quinidine half-life and corresponding AUC by about 50 to 60%. Quinidine concentrations should be monitored closely after one of these agents is added. No special precautions appear necessary if these agents are begun several weeks before quinidine is added but quinidine doses may require adjustment if one of these agents is added or discontinued during quinidine therapy.
Diazepam: (Moderate) Additive CNS and/or respiratory depression may occur. Additionally, barbiturates may increase the metabolism of diazepam. Diazepam is a CYP2C9, CYP2C19, and CYP3A4 substrate. Barbiturates are CYP2C9, CYP2C19, and CYP3A4 inducers.
Diclofenac: (Moderate) Caution is advised when administering diclofenac with inducers of CYP2C9, such as barbiturates. When used together, the systemic exposure to diclofenac (a CYP2C9 substrate) may decrease, potentially resulting in impaired efficacy. Higher diclofenac doses may be needed. In addition, phenobarbital toxicity has been reported to have occurred in a patient on chronic phenobarbital treatment after diclofenac initiation.
Diclofenac; Misoprostol: (Moderate) Caution is advised when administering diclofenac with inducers of CYP2C9, such as barbiturates. When used together, the systemic exposure to diclofenac (a CYP2C9 substrate) may decrease, potentially resulting in impaired efficacy. Higher diclofenac doses may be needed. In addition, phenobarbital toxicity has been reported to have occurred in a patient on chronic phenobarbital treatment after diclofenac initiation.
Dienogest; Estradiol valerate: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Diethylpropion: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants.
Diethylstilbestrol, DES: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Diflunisal: (Moderate) Acetaminophen plasma concentrations can increase by approximately 50% following administration of diflunisal. Acetaminophen has no effect on diflunisal concentrations. Acetaminophen in high doses has been associated with severe hepatotoxic reactions; therefore, caution should be exercised when using these agents concomitantly.
Dihydrocodeine; Guaifenesin; Pseudoephedrine: (Major) Concomitant use of dihydrocodeine with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when dihydrocodeine is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of dihydrocodeine with a barbiturate can decrease dihydrocodeine concentrations, resulting in less metabolism by CYP2D6 and decreased dihydromorphine concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of dihydrocodeine and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4, an isoenzyme partially responsible for the metabolism of dihydrocodeine. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Diltiazem: (Major) Diltiazem is a CYP3A4 substrate. Coadministration of diltiazem with known CYP3A4 inducers, such as barbiturates, may significantly decrease the bioavailability of diltiazem. When possible, avoid coadministration of these drugs and consider alternative therapy. When an alternative therapy is not possible, patients should be monitored for the desired cardiovascular effects on heart rate, chest pain, or blood pressure.
Dimenhydrinate: (Moderate) Additive CNS depression may occur if barbiturates are used concomitantly with dimenhydrinate.
Diphenhydramine: (Major) Because diphenhydramine can cause pronounced sedation, an enhanced CNS depressant effect may occur when it is combined with other CNS depressants including anxiolytics, sedatives, and hypnotics, such as barbiturates.
Diphenhydramine; Hydrocodone; Phenylephrine: (Major) Because diphenhydramine can cause pronounced sedation, an enhanced CNS depressant effect may occur when it is combined with other CNS depressants including anxiolytics, sedatives, and hypnotics, such as barbiturates. (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Diphenhydramine; Ibuprofen: (Major) Because diphenhydramine can cause pronounced sedation, an enhanced CNS depressant effect may occur when it is combined with other CNS depressants including anxiolytics, sedatives, and hypnotics, such as barbiturates.
Diphenhydramine; Naproxen: (Major) Because diphenhydramine can cause pronounced sedation, an enhanced CNS depressant effect may occur when it is combined with other CNS depressants including anxiolytics, sedatives, and hypnotics, such as barbiturates.
Diphenhydramine; Phenylephrine: (Major) Because diphenhydramine can cause pronounced sedation, an enhanced CNS depressant effect may occur when it is combined with other CNS depressants including anxiolytics, sedatives, and hypnotics, such as barbiturates. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Dipyridamole: (Major) Methylxanthines, through antagonism of adenosine and thus pharmacologic-induced coronary vasodilation, have been associated with false-negative results during dipyridamole-thallium 201 stress testing. It is recommended that methylxanthines (caffeine, caffeinated beverages and foods, theophylline, etc.) be discontinued for at least 24 hours prior to stress testing. An interaction is not expected when methylxanthines are used concomitantly with chronic dipyridamole therapy.
Disopyramide: (Moderate) Hepatic microsomal enzyme-inducing agents, such as barbiturates, have the potential to accelerate the hepatic metabolism of disopyramide, a CYP3A4 substrate. Serum disopyramide concentrations should be monitored closely if hepatic enzyme inducers are either added or discontinued during disopyramide therapy.
Disulfiram: (Moderate) Disulfiram has been shown to inhibit caffeine elimination. Caffeine elimination decreased by 30 percent in those patients that were not recovering alcoholics and by 24 percent in those patients that were recovering alcoholics. During disulfiram therapy, patients may need to limit their caffeine intake if nausea, nervousness, tremor, restlessness, palpitations, or insomnia complaints occur. Adverse events were not noted during this pharmacokinetic study, however, the decrease in caffeine clearance could be significant in some patients, including some patients with cardiovascular disease.
Dobutamine: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants.
Dolutegravir; Rilpivirine: (Moderate) Close clinical monitoring is advised when administering barbiturates with rilpivirine due to the potential for rilpivirine treatment failure. Although this interaction has not been studied, predictions can be made based on metabolic pathways. Barbiturates are inducers of the hepatic isoenzyme CYP3A4; rilpivirine is metabolized by this isoenzyme. Coadministration may result in decreased rilpivirine serum concentrations and impaired virologic response.
Donepezil: (Moderate) The elimination of donepezil may be increased by concurrent administration of moderate to strong inducers of CYP2D6 and CYP3A4, such as barbiturates (including primidone). The clinical effect of this interaction on the efficacy of donepezil has not been determined. Observe patients for evidence of reduced donepezil efficacy if these agents are prescribed concurrently.
Donepezil; Memantine: (Moderate) The elimination of donepezil may be increased by concurrent administration of moderate to strong inducers of CYP2D6 and CYP3A4, such as barbiturates (including primidone). The clinical effect of this interaction on the efficacy of donepezil has not been determined. Observe patients for evidence of reduced donepezil efficacy if these agents are prescribed concurrently.
Dopamine: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants.
Doravirine: (Moderate) Concurrent administration of doravirine and butalbital may result in decreased doravirine exposure, resulting in potential loss of virologic control. Doravirine is a CYP3A4 substrate; butalbital is a moderate CYP3A4 inducer.
Doravirine; Lamivudine; Tenofovir disoproxil fumarate: (Moderate) Concurrent administration of doravirine and butalbital may result in decreased doravirine exposure, resulting in potential loss of virologic control. Doravirine is a CYP3A4 substrate; butalbital is a moderate CYP3A4 inducer.
Doxercalciferol: (Moderate) Although these interactions have not been specifically studied, hepatic enzyme inducers, such as barbiturates, may affect the 25-hydroxylation of doxercalciferol and may necessitate dosage adjustments of doxercalciferol.
Doxorubicin: (Major) Barbiturates induce CYP3A4 and doxorubicin is a major substrate of CYP3A4. Inducers of CYP3A4 may decrease the concentration of doxorubicin and compromise the efficacy of chemotherapy. Avoid coadministration of barbiturates and doxorubicin if possible. If not possible, monitor doxorubicin closely for efficacy.
Doxycycline: (Major) Phenobarbital has been shown to affect the pharmacokinetics of doxycycline. Doxycycline half-life was decreased from 15.3 hours to 11.1 hours. It is likely that other barbiturates may exert the same effect. Clinicians should keep in mind that larger doses of doxycycline may be necessary in patients receiving barbiturates. This interaction may not apply to other tetracyclines since they are less dependent on hepatic metabolism for elimination.
Doxylamine: (Moderate) Because doxylamine can cause pronounced sedation, an enhanced CNS depressant effect may occur when it is combined with other CNS depressants including anxiolytics, sedatives, and hypnotics, such as barbiturates.
Doxylamine; Pyridoxine: (Moderate) Because doxylamine can cause pronounced sedation, an enhanced CNS depressant effect may occur when it is combined with other CNS depressants including anxiolytics, sedatives, and hypnotics, such as barbiturates.
Dronabinol: (Moderate) Use caution if coadministration of dronabinol with barbiturates is necessary, and monitor for an increase in barbiturate-related adverse reactions and a decrease in the efficacy of dronabinol. Additive dizziness, confusion, somnolence, and other CNS effects may also occur. Dronabinol is a CYP2C9 and 3A4 substrate; barbiturates are moderate or strong (phenobarbital) inducers of CYP3A4; additionally phenobarbital is a moderate CYP2C9 inducer. Concomitant use may result in decreased plasma concentrations of dronabinol. Decreased clearance of barbiturates has also been reported with dronabinol use, possibly by competitive inhibition of metabolism. Published data show an increase in the elimination half-life of pentobarbital by 4 hours when concomitantly dosed with dronabinol.
Dronedarone: (Major) The concomitant use of dronedarone and CYP3A4 inducers should be avoided. Dronedarone is metabolized by CYP3A. Barbiturates induce CYP3A4. Coadministration of CYP3A4 inducers, such as barbiturates, with dronedarone may result in reduced plasma concentration and subsequent reduced effectiveness of dronedarone therapy.
Droperidol: (Major) Central nervous system depressants, such as barbiturates, have additive or potentiating effects with droperidol. Following administration of droperidol, lower doses of the other CNS depressant should be used.
Drospirenone; Estradiol: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Drospirenone; Ethinyl Estradiol: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Drospirenone; Ethinyl Estradiol; Levomefolate: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Dyphylline: (Major) Due to the risk for additive adverse effects, avoid the concurrent administration of caffeine and dyphylline-containing products when possible. Concurrent administration can produce excessive xanthine-related adverse events such as nausea, irritability, nervousness, and insomnia. More severe adverse effects such as tremors, seizures, or cardiac arrhythmias are also possible with excessive dosages and in sensitive patients. In addition, counsel patients to limit dietary caffeine intake while taking dyphylline.
Dyphylline; Guaifenesin: (Major) Due to the risk for additive adverse effects, avoid the concurrent administration of caffeine and dyphylline-containing products when possible. Concurrent administration can produce excessive xanthine-related adverse events such as nausea, irritability, nervousness, and insomnia. More severe adverse effects such as tremors, seizures, or cardiac arrhythmias are also possible with excessive dosages and in sensitive patients. In addition, counsel patients to limit dietary caffeine intake while taking dyphylline.
Echinacea: (Moderate) Echinacea may inhibit the metabolism of caffeine. Echinacea reduces the oral clearance of caffeine by 27 percent and increases the mean AUC by 129 percent. Monitor patients for signs of increased caffeine serum concentrations if these drugs are coadministered until more data are available.
Efavirenz: (Major) Complex interactions may occur when barbiturates (e.g., phenobarbital) are administered to patients receiving treatment for HIV infection; if treating seizure disorder, a different anticonvulsant should be used whenever possible. If a barbiturate must be used in a patient being treated for HIV, the patient must be closely monitored for antiviral efficacy and seizure control; appropriate dose adjustments to the barbiturate or the antiretroviral medications are unknown. The combination regimens used to treat HIV often include substrates, inducers, and inhibitors of several CYP isoenzymes. Efavirenz is a substrate and inducer of CYP3A4 and an inhibitor of CYP2C9 and CYP2C19. Phenobarbital is an inducer of CYP3A4, and a substrate and inducer of CYP2C9 and CYP2C19. Use caution if these drugs are to be coadministered, with increased monitoring of both efavirenz and barbiturate concentrations. (Minor) Drugs that induce the hepatic isoenzymes CYP2E1 and CYP1A2, such as efavirenz, may potentially increase the risk for acetaminophen-induced hepatotoxicity via generation of a greater percentage of acetaminophen’s hepatotoxic metabolite, NAPQI. Also, the analgesic activity of acetaminophen may be reduced.
Efavirenz; Emtricitabine; Tenofovir: (Major) Complex interactions may occur when barbiturates (e.g., phenobarbital) are administered to patients receiving treatment for HIV infection; if treating seizure disorder, a different anticonvulsant should be used whenever possible. If a barbiturate must be used in a patient being treated for HIV, the patient must be closely monitored for antiviral efficacy and seizure control; appropriate dose adjustments to the barbiturate or the antiretroviral medications are unknown. The combination regimens used to treat HIV often include substrates, inducers, and inhibitors of several CYP isoenzymes. Efavirenz is a substrate and inducer of CYP3A4 and an inhibitor of CYP2C9 and CYP2C19. Phenobarbital is an inducer of CYP3A4, and a substrate and inducer of CYP2C9 and CYP2C19. Use caution if these drugs are to be coadministered, with increased monitoring of both efavirenz and barbiturate concentrations. (Minor) Drugs that induce the hepatic isoenzymes CYP2E1 and CYP1A2, such as efavirenz, may potentially increase the risk for acetaminophen-induced hepatotoxicity via generation of a greater percentage of acetaminophen’s hepatotoxic metabolite, NAPQI. Also, the analgesic activity of acetaminophen may be reduced.
Efavirenz; Lamivudine; Tenofovir Disoproxil Fumarate: (Major) Complex interactions may occur when barbiturates (e.g., phenobarbital) are administered to patients receiving treatment for HIV infection; if treating seizure disorder, a different anticonvulsant should be used whenever possible. If a barbiturate must be used in a patient being treated for HIV, the patient must be closely monitored for antiviral efficacy and seizure control; appropriate dose adjustments to the barbiturate or the antiretroviral medications are unknown. The combination regimens used to treat HIV often include substrates, inducers, and inhibitors of several CYP isoenzymes. Efavirenz is a substrate and inducer of CYP3A4 and an inhibitor of CYP2C9 and CYP2C19. Phenobarbital is an inducer of CYP3A4, and a substrate and inducer of CYP2C9 and CYP2C19. Use caution if these drugs are to be coadministered, with increased monitoring of both efavirenz and barbiturate concentrations. (Minor) Drugs that induce the hepatic isoenzymes CYP2E1 and CYP1A2, such as efavirenz, may potentially increase the risk for acetaminophen-induced hepatotoxicity via generation of a greater percentage of acetaminophen’s hepatotoxic metabolite, NAPQI. Also, the analgesic activity of acetaminophen may be reduced.
Elbasvir; Grazoprevir: (Severe) Concurrent administration of barbiturates with elbasvir; grazoprevir is contraindicated. Barbiturates are strong CYP3A inducers, while both elbasvir and grazoprevir are substrates of CYP3A. Use of these drugs together is expected to significantly decrease the plasma concentrations of both elbasvir and grazoprevir, and may result in decreased virologic response.
Eltrombopag: (Moderate) Eltrombopag is a UDP-glucuronyltransferase inhibitor. Acetaminophen is a substrate of UDP-glucuronyltransferases. The significance or effect of this interaction is not known; however, elevated concentrations of acetaminophen are possible. Monitor patients for adverse reactions if these drugs are coadministered. (Moderate) Eltrombopag is metabolized by CYP1A2. The significance of administering inducers of CYP1A2, such as barbiturates, on the systemic exposure of eltrombopag has not been established. Monitor patients for a decrease in the efficacy of eltrombopag if these drugs are coadministered.
Empagliflozin; Linagliptin: (Major) Inducers of CYP3A4 (e.g., barbiturates) can decrease exposure to linagliptin to subtherapeutic and likely ineffective concentrations. For patients requiring use of such drugs, an alternative to linagliptin is strongly recommended.
Emtricitabine; Rilpivirine; Tenofovir alafenamide: (Moderate) Close clinical monitoring is advised when administering barbiturates with rilpivirine due to the potential for rilpivirine treatment failure. Although this interaction has not been studied, predictions can be made based on metabolic pathways. Barbiturates are inducers of the hepatic isoenzyme CYP3A4; rilpivirine is metabolized by this isoenzyme. Coadministration may result in decreased rilpivirine serum concentrations and impaired virologic response.
Emtricitabine; Rilpivirine; Tenofovir disoproxil fumarate: (Moderate) Close clinical monitoring is advised when administering barbiturates with rilpivirine due to the potential for rilpivirine treatment failure. Although this interaction has not been studied, predictions can be made based on metabolic pathways. Barbiturates are inducers of the hepatic isoenzyme CYP3A4; rilpivirine is metabolized by this isoenzyme. Coadministration may result in decreased rilpivirine serum concentrations and impaired virologic response.
Enalapril; Felodipine: (Major) Barbiturates (e.g., phenobarbital, primidone) may significantly reduce systemic exposure of felodipine; consider alternative therapy. If coadministration is necessary, monitor the patient closely for desired cardiovascular effects on heart rate, blood pressure, or chest pain. Felodipine is a CYP3A4 substrate, and these anticonvulsants are potent CYP3A4 inducers. In a pharmacokinetic study, felodipine’s Cmax was considerably lower in epileptic patients on long-term anticonvulsant therapy than in healthy volunteers. In these patients, the mean AUC was reduced approximately 6% of that observed in healthy adults.
Enalapril; Hydrochlorothiazide, HCTZ: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Encorafenib: (Major) Avoid coadministration of encorafenib and butalbital due to decreased encorafenib exposure and potential loss of efficacy. Encorafenib is a CYP3A4 substrate; butalbital is a moderate CYP3A4 inducer. Coadministration with CYP3A4 inducers has not been studied with encorafenib; however, in clinical trials, steady-state encorafenib exposures were lower than encorafenib exposures after the first dose, suggesting CYP3A4 auto-induction.
Entacapone: (Moderate) COMT inhibitors, like entacapone or tolcapone, should be given cautiously with other agents that cause CNS depression due to the possibility of additive sedation. Agents that may cause additive sedation when given concurrently with tolcapone include the barbiturates. The risk for adverse effects may increase, and patients should use caution in driving or other hazardous tasks until the effects of the drugs are known.
Entrectinib: (Major) Avoid coadministration of entrectinib with butalbital due to decreased entrectinib exposure and risk of decreased efficacy. Entrectinib is a CYP3A4 substrate; butalbital is a moderate CYP3A4 inducer. Coadministration of a moderate CYP3A4 inducer is predicted to reduce the entrectinib AUC by 56%.
Ephedrine: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants like ephedrine. Adverse effects such as nervousness, irritability, insomnia, and/or cardiac arrhythmias are also possible when excessive dosages of caffeine are taken concurrently with ephedrine. Patients may also need to limit their intake of caffeine-containing beverages or foods (e.g., coffee, green tea, other teas, guarana, colas, or chocolate) to avoid caffeine-like side effects.
Epinephrine: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants.
Eprosartan; Hydrochlorothiazide, HCTZ: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Erdafitinib: (Major) If coadministration of erdafitinib and butalbital is necessary at the initiation of erdafitinib therapy, administer the dose of erdafitinib as recommended (8 mg once daily with potential to increase the dose to 9 mg on days 14 to 21 based on phosphate levels and tolerability). If butalbital must be added to erdafitinib therapy after the initial dose increase period (days 14 to 21), increase the dose of erdafitinib up to 9 mg. If butalbital is discontinued, continue erdafitinib at the same dose in the absence of drug-related toxicity. Erdafitinib is a CYP3A4 substrate and butalbital is a moderate CYP3A4 inducer.
Erlotinib: (Moderate) There may be a risk of reduced erlotinib efficacy when coadministered with butalbital; however, the risk has not been clearly defined. If coadministration is necessary, consider increasing the erlotinib dose by 50 mg increments at 2-week intervals as tolerated, to a maximum of 450 mg. Erlotinib is primarily metabolized by CYP3A4, and to a lesser extent by CYP1A2. Butalbital is a CYP3A4 and 1A2 inducer. Coadministration may decrease plasma concentrations of erlotinib.
Erythromycin: (Moderate) Inhibitors of the hepatic CYP4501A2, such as erythromycin, may inhibit the hepatic oxidative metabolism of caffeine. No specific management is recommended except in patients who complain of caffeine related side effects. In such patients, the dosage of caffeine containing medications or the ingestion of caffeine containing products may need to be reduced.
Erythromycin; Sulfisoxazole: (Moderate) Inhibitors of the hepatic CYP4501A2, such as erythromycin, may inhibit the hepatic oxidative metabolism of caffeine. No specific management is recommended except in patients who complain of caffeine related side effects. In such patients, the dosage of caffeine containing medications or the ingestion of caffeine containing products may need to be reduced.
Escitalopram: (Moderate) Escitalopram is metabolized by CYP2C19 and CYP3A4. Barbiturates can induce the metabolism of various CYP 450 isoenzymes, including those involved in escitalopram metabolism. Although no clinical data are available to support a clinically significant interaction, escitalopram may need to be administered in higher doses in patients chronically taking barbiturates.
Esketamine: (Major) Closely monitor blood pressure during concomitant use of esketamine and caffeine. Coadministration of psychostimulants, such as caffeine, with esketamine may increase blood pressure. (Major) Closely monitor patients receiving esketamine and barbiturates for sedation and other CNS depressant effects. Instruct patients who receive a dose of esketamine not to drive or engage in other activities requiring alertness until the next day after a restful sleep.
Eslicarbazepine: (Major) Barbiturates may induce the metabolism of eslicarbazepine resulting in decreased plasma concentrations of and potentially reduced efficacy of eslicarbazepine. An increased dose of eslicarbazepine may be necessary if these drugs are coadministered.
Esomeprazole: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19.
Esomeprazole; Naproxen: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19.
Estazolam: (Moderate) Additive CNS and/or respiratory depression may occur. Additionally, barbiturates may increase the metabolism of estazolam. Estazolam is a CYP3A4 substrate. Barbiturates are CYP3A4 inducers.
Esterified Estrogens: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Esterified Estrogens; Methyltestosterone: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Estradiol Cypionate; Medroxyprogesterone: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Estradiol: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Estradiol; Levonorgestrel: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Estradiol; Norethindrone: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Estradiol; Norgestimate: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Estradiol; Progesterone: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Estrogens: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Estropipate: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Eszopiclone: (Major) Barbiturates are potent inducers of CYP3A4 may increase the rate of eszopiclone metabolism. Additive CNS depression may also occur if barbiturates are used concomitantly with eszopiclone. Caution should be exercised during concomitant use of eszopiclone and any barbiturate; dosage reduction of one or both agents may be necessary. (Minor) Patients taking eszopiclone for sleep should avoid caffeine-containing medications, dietary supplements, foods, and beverages close to bedtime, as well as excessive total daily caffeine intake, as part of proper sleep hygiene, since caffeine intake can interfere with proper sleep. Limit use of caffeine-containing products including medications, dietary supplements (e.g., guarana), and beverages (e.g., coffee, green tea, other teas, or colas).
Ethanol: (Major) Alcohol is associated with CNS depression. The combined use of alcohol and CNS depressants can lead to additive CNS depression, which could be dangerous in tasks requiring mental alertness and fatal in overdose. Alcohol taken with other CNS depressants can lead to additive respiratory depression, hypotension, profound sedation, or coma. Consider the patient’s use of alcohol or illicit drugs when prescribing CNS depressant medications. In many cases, the patient should receive a lower dose of the CNS depressant initially if the patient is not likely to be compliant with avoiding alcohol. (Major) The risk of developing hepatotoxicity from acetaminophen appears to be increased in patients who regularly consume ethanol. Patients who drink more than 3 alcoholic drinks a day and take acetaminophen are at increased risk of developing hepatotoxicity. Acute or chronic ethanol use increases acetaminophen-induced hepatotoxicity by inducing cytochrome P450 CYP 2E1 leading to increased formation of the hepatotoxic metabolite of acetaminophen. Also, chronic alcohol use can deplete liver glutathione stores. Administration of acetaminophen should be limited or avoided altogether in patients with alcoholism or patients who consume ethanol regularly.
Ethinyl Estradiol: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethinyl Estradiol; Desogestrel: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethinyl Estradiol; Ethynodiol Diacetate: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethinyl Estradiol; Etonogestrel: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethinyl Estradiol; Levonorgestrel: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethinyl Estradiol; Levonorgestrel; Ferrous bisglycinate: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethinyl Estradiol; Levonorgestrel; Folic Acid; Levomefolate: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethinyl Estradiol; Norelgestromin: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethinyl Estradiol; Norethindrone Acetate: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethinyl Estradiol; Norethindrone Acetate; Ferrous fumarate: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethinyl Estradiol; Norethindrone: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethinyl Estradiol; Norethindrone; Ferrous fumarate: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethinyl Estradiol; Norgestimate: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethinyl Estradiol; Norgestrel: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Ethosuximide: (Moderate) Barbiturates induce hepatic microsomal enzymes and increase the hepatic metabolism of ethosuximide, leading to a decrease in ethosuximide plasma concentrations and half-life. To maintain a therapeutic dosage, serum concentrations of ethosuximide should be measured, especially if barbiturate therapy is added to or withdrawn from ethosuximide therapy.
Etoposide, VP-16: (Major) Monitor for clinical efficacy of etoposide, VP-16 when coadministered with butalbital, as concomitant use may be associated with increased etoposide clearance and reduced efficacy. Barbiturates, such as butalbital, induce CYP3A4; etoposide is a CYP3A4 substrate.
Exenatide: (Minor) Although an interaction is possible, these drugs may be used together. To avoid potential pharmacokinetic interactions that might alter effectiveness of acetaminophen, it may be advisable for patients to take acetaminophen at least 1 hour prior to an exenatide injection. When 1,000 mg acetaminophen elixir was given with 10 mcg exenatide (at 0 hours) and at 1, 2 and 4 hours after exenatide injection, acetaminophen AUCs were decreased by 21%, 23%, 24%, and 14%, respectively; Cmax was decreased by 37%, 56%, 54%, and 41%, respectively. Additionally, acetaminophen Tmax was delayed from 0.6 hours in the control period to 0.9, 4.2, 3.3, and 1.6 hours, respectively. Acetaminophen AUC, Cmax, and Tmax were not significantly changed when acetaminophen was given 1 h before exenatide injection. The mechanism of this interaction is not available (although it may be due to delayed gastric emptying from exenatide use) and the clinical impact has not been assessed.
Ezetimibe; Simvastatin: (Moderate) Barbiturates are significant hepatic CYP3A4 inducers. Monitor for potential reduced cholesterol-lowering efficacy when barbiturates are co-administered with simvastatin, which is metabolized by CYP3A4.
Fedratinib: (Major) Avoid coadministration of fedratinib with butalbital as concurrent use may decrease fedratinib exposure which may result in decreased therapeutic response. Fedratinib is a CYP3A4 substrate; butalbital is a moderate CYP3A4 inducer. The coadministration of fedratinib with a moderate CYP3A4 inducer has not been evaluated.
Felodipine: (Major) Barbiturates (e.g., phenobarbital, primidone) may significantly reduce systemic exposure of felodipine; consider alternative therapy. If coadministration is necessary, monitor the patient closely for desired cardiovascular effects on heart rate, blood pressure, or chest pain. Felodipine is a CYP3A4 substrate, and these anticonvulsants are potent CYP3A4 inducers. In a pharmacokinetic study, felodipine’s Cmax was considerably lower in epileptic patients on long-term anticonvulsant therapy than in healthy volunteers. In these patients, the mean AUC was reduced approximately 6% of that observed in healthy adults.
Fenoprofen: (Minor) Phenobarbital and possibly other barbiturates can decrease the plasma concentrations and half-life of fenoprofen. The clinical significance of this interaction has not been established, but dosage adjustments of fenoprofen may be necessary with concurrent administration of phenobarbital or following initiation or withdrawal of the drug.
Fentanyl: (Major) Concomitant use of fentanyl with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concurrent use of fentanyl with a barbiturate may decrease fentanyl plasma concentrations, decrease opioid efficacy, and potentially lead to a withdrawal syndrome in those with physical dependence to opioid agonists. Monitor for signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of increased opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; fentanyl is a CYP3A4 substrate.
Fesoterodine: (Minor) Beverages containing caffeine or ethanol may aggravate bladder symptoms and counteract the effectiveness of fesoterodine to some degree. Patients may wish to limit their intake of caffeinated drugs, dietary supplements (e.g., guarana), or beverages (e.g., green tea, other teas, coffee, colas) and alcoholic beverages.
Fexofenadine; Pseudoephedrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Flibanserin: (Major) The concomitant use of flibanserin with CYP3A4 inducers significantly decreases flibanserin exposure compared to the use of flibanserin alone. Therefore, concurrent use of flibanserin and phenobarbital or other barbiturates, which are strong CYP3A4 inducers, is not recommended.
Fluconazole: (Moderate) Fluconazole has been shown to inhibit the clearance of caffeine by 25 percent. The clinical significance of these interactions has not been determined. (Minor) Barbiturates induce hepatic CYP enzymes including 3A4, 2C19 and 2C9 and may reduce effective serum concentrations of fluconazole. Be alert for lack of efficacy of fluconazole in concurrent use.
Fluoxetine; Olanzapine: (Moderate) Olanzapine is metabolized by the CYP1A2 hepatic microsomal isoenzyme, and inducers of this enzyme such as barbiturates, may increase olanzapine clearance. The clinical effect of this interaction is thought to be minimal; however, the clinician should be alert for reduced olanzapine effect if the drugs are coadministered. Additive effects are possible when olanzapine is combined with other drugs which cause respiratory depression and/or CNS depression. Barbiturates can cause CNS depression, and if used concomitantly with olanzapine, can increase both the frequency and the intensity of adverse effects such as drowsiness, sedation, dizziness, and orthostatic hypotension.
Fluticasone: (Moderate) Coadministration may result in decreased exposure to fluticasone. Butalbital is a CYP3A4 inducer; fluticasone is a CYP3A4 substrate. Monitor for decreased response to fluticasone during concurrent use.
Fluticasone; Salmeterol: (Moderate) Coadministration may result in decreased exposure to fluticasone. Butalbital is a CYP3A4 inducer; fluticasone is a CYP3A4 substrate. Monitor for decreased response to fluticasone during concurrent use. (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Fluticasone; Umeclidinium; Vilanterol: (Moderate) Coadministration may result in decreased exposure to fluticasone. Butalbital is a CYP3A4 inducer; fluticasone is a CYP3A4 substrate. Monitor for decreased response to fluticasone during concurrent use. (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Fluticasone; Vilanterol: (Moderate) Coadministration may result in decreased exposure to fluticasone. Butalbital is a CYP3A4 inducer; fluticasone is a CYP3A4 substrate. Monitor for decreased response to fluticasone during concurrent use. (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Fluvoxamine: (Moderate) Strong inhibitors of CYP1A2, such as fluvoxamine, may inhibit the metabolism of caffeine. No specific management is recommended except in patients with caffeine-related side effects after initiating fluvoxamine. In such patients, the dosage of caffeine containing medications or the ingestion of caffeine containing products may need to be reduced.
Food: (Moderate) The incidence of marijuana associated adverse effects may change following coadministration with barbiturates. Barbiturates are inducers of CYP2C9 and CYP3A4, two isoenzymes responsible for the metabolism of marijuana’s most psychoactive compound, delta-9-tetrahydrocannabinol (Delta-9-THC). When given concurrently with barbiturates, the amount of Delta-9-THC converted to the active metabolite 11-hydroxy-delta-9-tetrahydrocannabinol (11-OH-THC) may be increased. These changes in Delta-9-THC and 11-OH-THC plasma concentrations may result in an altered marijuana adverse event profile.
Formoterol: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Formoterol; Mometasone: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Fosamprenavir: (Major) Coadministration with phenobarbital and, potentially, other barbiturates may increase the metabolism of fosamprenavir and lead to decreased fosamprenavir concentrations resulting in reduction of antiretroviral efficacy and development of viral resistance. If fosamprenavir and barbiturates are used together, the patient must be closely monitored for antiviral efficacy.
Fosinopril; Hydrochlorothiazide, HCTZ: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Galantamine: (Moderate) Monitor for reduced efficacy of galantamine during concurrent use of barbiturates. Galantamine is a substrate for CYP3A4 and CYP2D6. The effectiveness of the drug could theoretically be reduced by the concomitant administration of strong CYP3A4 inducers such as barbiturates.
Gallium Ga 68 Dotatate: (Minor) Mannitol promotes the urinary excretion of barbiturates, and it may be used as an adjunct in patients with barbiturate toxicity.
General anesthetics: (Moderate) Additive CNS depression may occur if general anesthetics are used concomitantly with barbiturates.
Givosiran: (Major) Avoid concomitant use of givosiran and caffeine due to the risk of increased caffeine-related adverse reactions. If use is necessary, consider decreasing the caffeine dose. Caffeine is a sensitive CYP1A2 substrate. Givosiran may moderately reduce hepatic CYP1A2 enzyme activity because of its pharmacological effects on the hepatic heme biosynthesis pathway.
Glimepiride: (Minor) Barbiturates may induce the CYP2C9 metabolism of glimepiride. Blood glucose concentrations should be monitored and possible dose adjustments of glimepiride may need to be made.
Glimepiride; Pioglitazone: (Minor) Barbiturates may induce the CYP2C9 metabolism of glimepiride. Blood glucose concentrations should be monitored and possible dose adjustments of glimepiride may need to be made.
Glimepiride; Rosiglitazone: (Minor) Barbiturates may induce the CYP2C9 metabolism of glimepiride. Blood glucose concentrations should be monitored and possible dose adjustments of glimepiride may need to be made.
Glycopyrrolate; Formoterol: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Grapefruit juice: (Minor) Data are limited and conflicting as to whether grapefruit juice significantly alters the serum concentrations and/or AUC of caffeine. Caffeine is primarily a CYP1A2 substrate, and grapefruit juice appears to have but a small effect on this enzyme in vivo. One report suggests that grapefruit juice decreases caffeine elimination by inhibition of flavin-containing monooxygenase, a P450 independent system. This interaction might increase caffeine levels and mildly potentiate the clinical effects and common side effects of caffeine. If side effects appear, patients may need to limit either caffeine or grapefruit juice intake.
Green Tea: (Moderate) Many green tea products contain caffeine. Due to the risk for adverse effects, avoid the concurrent administration of caffeine and green tea products that contain caffeine when possible. Concurrent administration can produce excessive caffeine-related adverse events such as nausea, irritability, nervousness, and insomnia. (Minor) Some green tea products contain caffeine. The metabolism of xanthines, such as caffeine, can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Griseofulvin: (Minor) Barbiturates can impair the oral absorption of griseofulvin, resulting in decreased serum concentrations and, potentially, decreased antifungal efficacy. The clinical significance of this interaction is uncertain, but the manufacturer recommends that these drugs not be co-administered.
Guaifenesin; Hydrocodone: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate.
Guaifenesin; Hydrocodone; Pseudoephedrine: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Guaifenesin; Phenylephrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Guaifenesin; Pseudoephedrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Guanfacine: (Major) Monitor patients for guanfacine efficacy and for excess sedation during butalbital coadministration. Guanfacine plasma concentrations can be reduced by butalbital, by induction of CYP3A4 metabolism. Immediate-release guanfacine may require more frequent dosing to achieve or maintain desired hypotensive response; if it is discontinued, carefully taper the dose to prevent rebound hypertension. The extended-release guanfacine dose for attention deficit hyperactivity disorder (ADHD) may need to be doubled, per FDA-approved labeling; any dose change should occur over 1 to 2 weeks (e.g., dose increase when adding, or decrease when discontinuing, an enzyme inducer). Guanfacine is primarily metabolized by CYP3A4. Barbiturates (e.g., phenobarbital, primidone) are strong CYP3A4 inducers. Guanfacine plasma concentrations and elimination half-life were significantly reduced with coadministration of an enzyme inducer (e.g., phenobarbital, primidone, phenytoin, fosphenytoin) in two patients with renal impairment. Additionally, guanfacine has been associated with sedative effects and can potentiate the actions of CNS depressants, including barbiturates.
Haloperidol: (Moderate) Haloperidol can potentiate the actions of other CNS depressants such as barbiturates. Caution should be exercised with simultaneous use of these agents due to potential excessive CNS effects.
Hemin: (Major) Hemin works by inhibiting the enzyme (delta)-aminolevulinic acid synthetase. Drugs which increase the activity of this enzyme, such as barbiturates should not be used with hemin.
Homatropine; Hydrocodone: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate.
Hydantoins: (Moderate) Barbiturates can stimulate the hydroxylating enzyme that metabolizes phenytoin or, conversely, may inhibit phenytoin (or fosphenytoin) metabolism. In general, therapeutic doses of phenobarbital induce the hepatic metabolism of phenytoin, producing lower phenytoin serum concentrations. Large doses of phenobarbital, however, tend to increase phenytoin serum concentrations due to competition for hepatic pathways. Thus, phenytoin serum concentrations can increase, decrease, or not change during concomitant therapy with barbiturates. Conversely, phenytoin can increase serum concentrations of the barbiturate, however this has not been as well studied. Similar interactions may occur with ethotoin, although specific data are lacking. (Minor) Hydantoin anticonvulsants induce hepatic microsomal enzymes and may increase the metabolism of other drugs, leading to reduced efficacy of medications like acetaminophen. In addition, the risk of hepatotoxicity from acetaminophen may be increased with the chronic dosing of acetaminophen along with phenytoin. Adhere to recommended acetaminophen dosage limits. Acetaminophen-related hepatotoxicity has occurred clinically with the concurrent use of acetaminophen 1300 mg to 6200 mg daily and phenytoin. Acetaminophen cessation led to serum transaminase normalization within 2 weeks. (Minor) The metabolism of caffeine, can be increased by concurrent use with medications that cause induction of hepatic CYP450 enzymes like the hydantoin anticonvulsants.
Hydralazine; Hydrochlorothiazide, HCTZ: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrochlorothiazide, HCTZ: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrochlorothiazide, HCTZ; Irbesartan: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrochlorothiazide, HCTZ; Lisinopril: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrochlorothiazide, HCTZ; Losartan: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrochlorothiazide, HCTZ; Methyldopa: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrochlorothiazide, HCTZ; Metoprolol: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrochlorothiazide, HCTZ; Moexipril: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrochlorothiazide, HCTZ; Olmesartan: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrochlorothiazide, HCTZ; Propranolol: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrochlorothiazide, HCTZ; Quinapril: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrochlorothiazide, HCTZ; Spironolactone: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics. (Moderate) Barbiturates, such as butalbital, may potentiate orthostatic hypotension when given concomitantly with spironolactone.
Hydrochlorothiazide, HCTZ; Telmisartan: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrochlorothiazide, HCTZ; Triamterene: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrochlorothiazide, HCTZ; Valsartan: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Hydrocodone: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate.
Hydrocodone; Ibuprofen: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate.
Hydrocodone; Phenylephrine: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Hydrocodone; Potassium Guaiacolsulfonate: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate.
Hydrocodone; Potassium Guaiacolsulfonate; Pseudoephedrine: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Hydrocodone; Pseudoephedrine: (Major) Concomitant use of hydrocodone with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. It is recommended to avoid this combination when hydrocodone is being used for cough. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of hydrocodone with a barbiturate can decrease hydrocodone concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of hydrocodone and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; hydrocodone is a CYP3A4 substrate. (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Hydromorphone: (Major) Concomitant use of hydromorphone with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation.
Hydroxyprogesterone: (Moderate) In vitro studies indicate that hydroxyprogesterone increases the metabolic rate of CYP2A6 isoenzymes. The metabolism of drugs metabolized by CYP2A6, such as acetaminophen may be increased during treatment with hydroxyprogesterone.
Hydroxyzine: (Major) Because hydroxyzine can cause pronounced sedation, an enhanced CNS depressant effect may occur when it is combined with other CNS depressants including barbiturates.
Hyoscyamine; Methenamine; Methylene Blue; Phenyl Salicylate; Sodium Biphosphate: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur.
Ibuprofen; Oxycodone: (Major) Concomitant use of oxycodone with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concurrent use of oxycodone with a barbiturate may decrease oxycodone plasma concentrations, decrease opioid efficacy, and potentially lead to a withdrawal syndrome in those with physical dependence to opioid agonists. Monitor for signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of increased opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; oxycodone is a CYP3A4 substrate.
Ibuprofen; Pseudoephedrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Ifosfamide: (Moderate) Closely monitor for increased ifosfamide-related toxicities (e.g., neurotoxicity, nephrotoxicity) if coadministration with butalbital is necessary; consider adjusting the dose of ifosfamide as clinically appropriate. Ifosfamide is metabolized to its active alkylating metabolites by CYP3A4; butalbital is a CYP3A4 inducer. Concomitant use may increase the formation of the neurotoxic/nephrotoxic ifosfamide metabolite, chloroacetaldehyde.
Iloperidone: (Moderate) Barbiturates can cause CNS depression, and if used concomitantly with iloperidone, may increase both the frequency and the intensity of adverse effects such as drowsiness, sedation, and dizziness. In theory, the use of barbiturates and iloperidone may also result in an increase in iloperidone elimination as a result of the CYP inducing effects of barbiturates.
Imatinib: (Major) Barbiturates induce CYP3A4 and may increase the metabolism of imatinib and decrease imatinib concentrations and clinical effects. Caution is recommended when imatinib is given in combination with barbiturates. (Major) Imatinib, STI-571 may affect the metabolism of acetaminophen. In vitro, imatinib was found to inhibit acetaminophen O-glucuronidation at therapeutic levels. Therefore, systemic exposure to acetaminophen is expected to be increased with coadministration of imatinib. Chronic acetaminophen therapy should be avoided in patients receiving imatinib.
Indacaterol: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Indacaterol; Glycopyrrolate: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Indinavir: (Major) Barbiturates may increase the metabolism of indinavir and lead to decreased antiretroviral efficacy. In addition, indinavir may inhibit the CYP metabolism of barbiturates, resulting in increased barbiturate concentrations. Appropriate dose adjustments necessary to ensure optimum levels of both anti-retroviral agent and the barbiturate are unknown. Anticonvulsant serum concentrations should be monitored closely if these agents are added; the patient should be observed for changes in the clinical efficacy of the antiretroviral or anticonvulsant regimen.
Insulin Glargine; Lixisenatide: (Minor) When 1,000 mg acetaminophen was given 1 or 4 hours after 10 mcg lixisenatide, the AUC was not significantly changed, but the acetaminophen Cmax was decreased by 29% and 31%, respectively and median Tmax was delayed by 2 and 1.75 hours, respectively. Acetaminophen AUC, Cmax, and Tmax were not significantly changed when acetaminophen was given 1 h before lixisenatide injection. The mechanism of this interaction is not available (although it may be due to delayed gastric emptying) and the clinical impact has not been assessed. To avoid potential pharmacokinetic interactions that might alter effectiveness of acetaminophen, it may be advisable for patients to take acetaminophen at least one hour prior to lixisenatide subcutaneous injection.
Isavuconazonium: (Moderate) Concomitant use of isavuconazonium with acetaminophen may result in increased serum concentrations of acetaminophen. Acetaminophen is a substrate of the hepatic isoenzyme CYP3A4; isavuconazole, the active moiety of isavuconazonium, is a moderate inhibitor of this enzyme. Caution and close monitoring are advised if these drugs are used together.
Isocarboxazid: (Major) Additive CNS depression may occur if butalbital is used concomitantly with monoamine oxidase inhibitors. (Major) Excessive use of caffeine in any form should be avoided in patients receiving Monoamine oxidase inhibitors (MAOIs). Limit caffeine intake during MAOI use and for 1 to 2 weeks after discontinuation of any MAOI. the use of non-prescription medicines or dietary supplements containing caffeine should be avoided. Patients should try to avoid or limit the intake of all items containing caffeine such as tea, coffee, chocolate, and cola. Cardiac arrhythmias or severe hypertension may occur because of the potentiation of caffeine’s sympathomimetic effects by MAOIs if caffeine intake is excessive. Ordinarily, selegiline may be an exception, it can only be used safely without dietary restrictions at doses where it presumably selectively inhibits MAO-B (e.g., 10 mg/day). At doses of 20 mg/day, selegiline can interact with foods and beverages. The precise dose at which selegiline becomes a non-selective inhibitor of all MAO is unknown, but may be in the range of 30 to 40 mg per day. Attention to the dose dependent nature of selegiline’s selectivity is critical if it is to be used without elaborate restrictions being placed on diet.
Isoniazid, INH: (Major) Agents which induce the hepatic isoenzyme CYP2E1, such as isoniazid, may potentially increase the risk for acetaminophen-induced hepatotoxicity via generation of a greater percentage of acetaminophen’s hepatotoxic metabolites. The combination of isoniazid and acetaminophen has caused severe hepatotoxicity in at least one patient; studies in rats have demonstrated that pre-treatment with isoniazid potentiates acetaminophen hepatotoxicity. (Moderate) Although isoniazid does not inhibit mitochondrial MAO, it does appear to inhibit plasma MAO. Dangerous cardiac arrhythmias or severe hypertension can occur because of the potentiation of caffeine’s sympathomimetic effects by MAOIs. Caffeine use should be minimized or avoided during and for 1 to 2 weeks after discontinuation of any MAOI.
Isoniazid, INH; Pyrazinamide, PZA; Rifampin: (Major) Agents which induce the hepatic isoenzyme CYP2E1, such as isoniazid, may potentially increase the risk for acetaminophen-induced hepatotoxicity via generation of a greater percentage of acetaminophen’s hepatotoxic metabolites. The combination of isoniazid and acetaminophen has caused severe hepatotoxicity in at least one patient; studies in rats have demonstrated that pre-treatment with isoniazid potentiates acetaminophen hepatotoxicity. (Moderate) Agents which induce the hepatic isoenzymes CYP2E1 and CYP1A2, such as rifampin, may potentially increase the risk for acetaminophen-induced hepatotoxicity via generation of a greater percentage of acetaminophen’s hepatotoxic metabolites. (Moderate) Although isoniazid does not inhibit mitochondrial MAO, it does appear to inhibit plasma MAO. Dangerous cardiac arrhythmias or severe hypertension can occur because of the potentiation of caffeine’s sympathomimetic effects by MAOIs. Caffeine use should be minimized or avoided during and for 1 to 2 weeks after discontinuation of any MAOI. (Moderate) It may be necessary to adjust the dosage of butalbital if given concurrently with rifampin. Rifampin may induce the metabolism of butalbital; coadministration may result in decreased butalbital plasma concentrations. (Minor) Rifampin is a potent inducer of the cytochrome P450 hepatic enzyme system and can reduce the plasma concentrations and possibly the efficacy of caffeine, including caffeine found in green tea products.
Isoniazid, INH; Rifampin: (Major) Agents which induce the hepatic isoenzyme CYP2E1, such as isoniazid, may potentially increase the risk for acetaminophen-induced hepatotoxicity via generation of a greater percentage of acetaminophen’s hepatotoxic metabolites. The combination of isoniazid and acetaminophen has caused severe hepatotoxicity in at least one patient; studies in rats have demonstrated that pre-treatment with isoniazid potentiates acetaminophen hepatotoxicity. (Moderate) Agents which induce the hepatic isoenzymes CYP2E1 and CYP1A2, such as rifampin, may potentially increase the risk for acetaminophen-induced hepatotoxicity via generation of a greater percentage of acetaminophen’s hepatotoxic metabolites. (Moderate) Although isoniazid does not inhibit mitochondrial MAO, it does appear to inhibit plasma MAO. Dangerous cardiac arrhythmias or severe hypertension can occur because of the potentiation of caffeine’s sympathomimetic effects by MAOIs. Caffeine use should be minimized or avoided during and for 1 to 2 weeks after discontinuation of any MAOI. (Moderate) It may be necessary to adjust the dosage of butalbital if given concurrently with rifampin. Rifampin may induce the metabolism of butalbital; coadministration may result in decreased butalbital plasma concentrations. (Minor) Rifampin is a potent inducer of the cytochrome P450 hepatic enzyme system and can reduce the plasma concentrations and possibly the efficacy of caffeine, including caffeine found in green tea products.
Isoproterenol: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants.
Isradipine: (Major) Because isradipine is a substrate of CYP3A4, the concomitant use of drugs that strongly induce CYP3A4, such as barbiturates, may cause a reduction in the bioavailability and thus decreased therapeutic effect of isradipine. Consider alternative therapy; if co-use is necessary, patients should be monitored for potential loss of therapeutic effect when hepatic enzyme inducers are added to isradipine therapy.
Itraconazole: (Major) Use of barbiturates is not recommended for 2 weeks before or during itraconazole therapy. Barbiturates induce hepatic CYP enzymes including 3A4, 2C19 and 2C9 and may reduce effective serum concentrations of itraconazole. Monitor for breakthrough fungal infections.
Ivabradine: (Major) Avoid coadministration of ivabradine and barbiturates including primidone. Ivabradine is primarily metabolized by CYP3A4; barbiturates induce CYP3A4. Coadministration may decrease the plasma concentrations of ivabradine resulting in the potential for treatment failure.
Ixabepilone: (Major) Ixabepilone is a CYP3A4 substrate and concomitant use with CYP3A4 inducers such as barbiturates may lead to reduced and subtherapeutic concentrations of ixabepilone. Caution should be utilized when CYP3A4 inducers are coadministered with ixabepilone, and alternative therapies with low enzyme induction potential should be considered.
Kava Kava, Piper methysticum: (Major) Kava kava should be avoided when possible in patients taking barbiturates. Additive sedation or other CNS-related side effects are possible. Kava may inhibit CYP enzymes, increasing barbiturate exposure. When available, therapeutic drug monitoring for the specific barbiturate (e.g., phenobarbital) may be advisable. Liver injury may occur with Kava, which may be an additive side effect with some barbiturate treatments.
Ketoconazole: (Moderate) Ketoconazole has been shown to inhibit the clearance of caffeine by 11 percent. The clinical significance of these interactions has not been determined. (Minor) Barbiturates induce hepatic CYP enzymes including 3A4, 2C19 and 2C9 and may reduce effective serum concentrations of ketoconazole. Clinicians should be alert for lack of efficacy of these antifungals in concurrent use.
Ketoprofen: (Minor) Caffeine administered concurrently with ketoprofen reduced the urine volume in 4 healthy volunteers. The clinical significance of the interaction in preterm neonates is not known.
Lamivudine, 3TC; Zidovudine, ZDV: (Minor) Both acetaminophen and zidovudine, ZDV undergo glucuronidation. Competition for the metabolic pathway is thought to have caused a case of acetaminophen-related hepatotoxicity. This interaction may be more clinically significant in patients with depleted glutathione stores, such as patients with acquired immunodeficiency syndrome, poor nutrition, or alcoholism.
Lamotrigine: (Major) Acetaminophen can be hepatotoxic, and lamotrigine appears to be a potential cause of progressive and fatal hepatotoxicity despite drug discontinuation. A 35 year-old developed fulminant liver failure possibly caused by lamotrigine. She was taking several other drugs including acetaminophen. In a randomized, single-dose study, the serum half-life of lamotrigine after a 300 mg dose decreased by 15% and the area under the plasma concentration-time curve decreased by 20% when given with acetaminophen 900 mg 3 times a day as compared with administration of lamotrigine with placebo. As the lamotrigine maximum serum concentration (Cmax) and time to Cmax was similar between the groups, and the lamotrigine renal clearance increased by 7%, acetaminophen appears to enhance removal of lamotrigine from the circulation.
Lansoprazole: (Moderate) Monitor for decreased efficacy of lansoprazole if concomitant use of lansoprazole and barbiturates is necessary. Lansoprazole is metabolized by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Drugs known to induce CYP3A4 and CYP2C19 may lead to decreased lansoprazole plasma concentrations.
Lansoprazole; Naproxen: (Moderate) Monitor for decreased efficacy of lansoprazole if concomitant use of lansoprazole and barbiturates is necessary. Lansoprazole is metabolized by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Drugs known to induce CYP3A4 and CYP2C19 may lead to decreased lansoprazole plasma concentrations.
Lanthanum Carbonate: (Minor) The manufacturer recommends that oral compounds known to interact with antacids, such as acetaminophen, should not be taken within 2 hours of dosing with lanthanum carbonate.
Lefamulin: (Major) Avoid coadministration of lefamulin with butalbital unless the benefits outweigh the risks as concurrent use may decrease lefamulin exposure and efficacy. Lefamulin is a CYP3A4 substrate; butalbital is a moderate CYP3A4 inducer.
Lesinurad: (Moderate) Barbiturates may decrease the systemic exposure and therapeutic effect of lesinurad; monitor for potential reduction in efficacy. Barbiturates induce the CYP2C9 isoenzyme, and lesinurad is a CYP2C9 substrate.
Lesinurad; Allopurinol: (Moderate) Barbiturates may decrease the systemic exposure and therapeutic effect of lesinurad; monitor for potential reduction in efficacy. Barbiturates induce the CYP2C9 isoenzyme, and lesinurad is a CYP2C9 substrate.
Leucovorin: (Minor) Limited data suggest that leucovorin and levoleucovorin may interfere with the activity of anticonvulsants such as barbiturates. Folic acid can decrease serum concentrations of anticonvulsants in children. Leucovorin shares metabolic pathways with folic acid. Clinicians should consider careful monitoring of patients.
Levalbuterol: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Levobupivacaine: (Minor) Barbiturates may induce the metabolism of levobupivacaine resulting in a decreased serum half-life. Dosage adjustments of levobupivacaine may be necessary.
Levocetirizine: (Moderate) Concurrent use of cetirizine/levocetirizine with barbiturates should generally be avoided. Coadministration may increase the risk of CNS depressant-related side effects. If concurrent use is necessary, monitor for excessive sedation and somnolence.
Levoleucovorin: (Minor) Limited data suggest that leucovorin and levoleucovorin may interfere with the activity of anticonvulsants such as barbiturates. Folic acid can decrease serum concentrations of anticonvulsants in children. Leucovorin shares metabolic pathways with folic acid. Clinicians should consider careful monitoring of patients.
Levorphanol: (Major) Concomitant use of levorphanol with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Reduce the initial dose of levorphanol by approximately 50% or more. Educate patients about the risks and symptoms of respiratory depression and sedation.
Lidocaine: (Moderate) Coadministration of lidocaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue lidocaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
Linagliptin: (Major) Inducers of CYP3A4 (e.g., barbiturates) can decrease exposure to linagliptin to subtherapeutic and likely ineffective concentrations. For patients requiring use of such drugs, an alternative to linagliptin is strongly recommended.
Linagliptin; Metformin: (Major) Inducers of CYP3A4 (e.g., barbiturates) can decrease exposure to linagliptin to subtherapeutic and likely ineffective concentrations. For patients requiring use of such drugs, an alternative to linagliptin is strongly recommended.
Linezolid: (Moderate) Caffeine use should be minimized or avoided during and for 1 to 2 weeks after discontinuation of linezolid. Linezolid is an antibiotic that is also a weak, reversible nonselective inhibitor of monoamine oxidase (MAO). Dangerous cardiac arrhythmias or severe hypertension can occur because of the potentiation of caffeine’s sympathomimetic effects by MAOIs.
Lisdexamfetamine: (Moderate) Avoid excessive caffeine intake during use of lisdexamfetamine. Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants. Excessive caffeine ingestion (via medicines, foods like chocolate, dietary supplements, or beverages including coffee, green tea, other teas, colas) may contribute to side effects like nervousness, irritability, nausea, insomnia, or tremor. Patients should avoid medications and dietary supplements which contain high amounts of caffeine.
Lithium: (Major) Caffeine appears to reduce serum lithium concentrations. Adverse reactions to lithium have also been noted to increase simultaneously with a reduction in caffeine intake. Patients taking lithium should be counseled regarding their intake of caffeine. (Moderate) Because lithium has the potential to impair cognitive and motor skills, caution is advisable during concurrent use of other medications with centrally-acting effects including anxiolytics, sedatives, and hypnotics.
Lixisenatide: (Minor) When 1,000 mg acetaminophen was given 1 or 4 hours after 10 mcg lixisenatide, the AUC was not significantly changed, but the acetaminophen Cmax was decreased by 29% and 31%, respectively and median Tmax was delayed by 2 and 1.75 hours, respectively. Acetaminophen AUC, Cmax, and Tmax were not significantly changed when acetaminophen was given 1 h before lixisenatide injection. The mechanism of this interaction is not available (although it may be due to delayed gastric emptying) and the clinical impact has not been assessed. To avoid potential pharmacokinetic interactions that might alter effectiveness of acetaminophen, it may be advisable for patients to take acetaminophen at least one hour prior to lixisenatide subcutaneous injection.
Lofexidine: (Moderate) Monitor for additive sedation during coadministration of lofexidine and barbiturates. Lofexidine can potentiate the effects of CNS depressants such as barbiturates. Patients should be advised to avoid driving or performing any other tasks requiring mental alertness until the effects of the combination are known. The use of barbiturates parenterally may cause vasodilation and an additive risk for hypotension and may lead to bradycardia and syncope; in these patients, careful monitoring of blood pressure should occur.
Lomitapide: (Moderate) Caution should be exercised when lomitapide is used with other medications known to have potential for hepatotoxicity, such as acetaminophen (> 4 g/day PO for >= 3 days/week). The effect of concomitant administration of lomitapide with other hepatotoxic medications is unknown. More frequent monitoring of liver-related tests may be warranted.
Lopinavir; Ritonavir: (Major) Barbiturates may increase the metabolism of lopinavir and lead to decreased antiretroviral efficacy. In addition, coadministration of lopinavir boosted with ritonavir may induce the CYP metabolism of barbiturates, resulting in decreased barbiturate concentrations. Appropriate dose adjustments necessary to ensure optimum levels of both anti-retroviral agent and the barbiturate are unknown; however, once daily lopinavir; ritonavir should not be used. Anticonvulsant serum concentrations should be monitored closely if these agents are added; the patient should be observed for changes in the clinical efficacy of the antiretroviral or anticonvulsant regimen. (Major) Concurrent use of ritonavir with phenobarbital or other barbiturates should be done cautiously. Increased doses of anticonvulsants may be required due metabolism induction by ritonavir. However, since these anticonvulsants are hepatic enzyme inducing drugs, increased metabolism of protease inhibitors may occur, leading to decreased antiretroviral efficacy. Close monitoring of drug concentrations and/or therapeutic and adverse effects is required. (Moderate) Concurrent administration of acetaminophen with ritonavir may result in elevated acetaminophen plasma concentrations and subsequent adverse events. Acetaminophen is metabolized by the hepatic isoenzyme CYP3A4; ritonavir is an inhibitor of this enzyme. Caution and close monitoring are advised if these drugs are administered together.
Loratadine; Pseudoephedrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Lorazepam: (Moderate) Additive CNS and/or respiratory depression may occur with concurrent use.
Lorlatinib: (Major) Avoid coadministration of lorlatinib with butalbital due to the potential for serious hepatotoxicity; the efficacy of lorlatinib may also be decreased. If concomitant use is unavoidable, monitor AST, ALT, and bilirubin 48 hours after initiating lorlatinib and at least 3 times during the first week after initiating lorlatinib. Monitor for changes in clinical response to lorlatinib. Depending upon the relative importance of each drug, discontinue lorlatinib or butalbital for persistent Grade 2 or higher hepatotoxicity. Lorlatinib is a CYP3A4 substrate and butalbital is a moderate CYP3A4 inducer. Severe hepatotoxicity occurred in healthy subjects receiving a single 100-mg dose of lorlatinib with multiple daily doses of a strong CYP3A4 inducer (n = 12); both drugs were also pregnane X receptor agonists (PXR). The effect of the concomitant use of moderate CYP3A inducers on lorlatinib pharmacokinetics or the risk of hepatotoxicity with the concomitant use of moderate CYP3A inducers is unknown.
Lovastatin: (Moderate) Barbiturates are significant hepatic CYP3A4 inducers. Monitor for potential reduced cholesterol-lowering efficacy when barbiturates are co-administered with HMG-CoA reductase inhibitors metabolized by CYP3A4 including lovastatin.
Lovastatin; Niacin: (Moderate) Barbiturates are significant hepatic CYP3A4 inducers. Monitor for potential reduced cholesterol-lowering efficacy when barbiturates are co-administered with HMG-CoA reductase inhibitors metabolized by CYP3A4 including lovastatin.
Loxapine: (Moderate) Loxapine can potentiate the actions of other CNS depressants, such as barbiturates. Caution should be exercised with simultaneous use of these agents due to potential excessive CNS effects.
Lurasidone: (Severe) Concurrent use of lurasidone with strong CYP3A4 inducers, such as barbiturates, is contraindicated. Lurasidone is primarily metabolized by CYP3A4. Decreased blood concentrations of lurasidone are expected when the drug is co-administered with strong inducers of CYP3A4.
Magnesium Salicylate: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. Although salicylates are rarely associated with nephrotoxicity, high-dose, chronic administration of salicylates combined other analgesics, including acetaminophen, significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Additive hepatic toxicity may occur, especially in combined overdose situations. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Magnesium Salts: (Minor) Because of the CNS-depressant effects of magnesium sulfate, additive central-depressant effects can occur following concurrent administration with CNS depressants such as barbiturates. Caution should be exercised when using these agents concurrently.
Mannitol: (Minor) Mannitol promotes the urinary excretion of barbiturates, and it may be used as an adjunct in patients with barbiturate toxicity.
Maprotiline: (Major) Monitor for excessive sedation and somnolence during coadministration maprotiline and barbiturates. Concurrent use may result in additive CNS depression.
Mebendazole: (Moderate) Barbiturates induce hepatic microsomal enzymes and may increase the metabolism of mebendazole if given concomitantly. This effect can cause decreased levels of plasma mebendazole but is probably important only in the treatment of extraintestinal infections, such as hydatid cyst disease, and not in the treatment of intestinal helminths.
Meclizine: (Moderate) Additive CNS depression may occur if barbiturates are used concomitantly with meclizine.
Mefloquine: (Moderate) The barbiturates induce CYP3A4 and may increase the metabolism of mefloquine if coadministered. Concomitant administration can reduce the clinical efficacy of mefloquine, increasing the risk of Plasmodium falciparum resistance during treatment of malaria. Coadministration of mefloquine and barbiturates that are used as anticonvulsants may also result in lower than expected anticonvulsant concentrations and loss of seizure control. Monitoring of the anticonvulsant serum concentration, if the drug is monitored via therapeutic drug monitoring, is recommended. Mefloquine may cause CNS side effects that may cause seizures or alter moods or behaviors.
Melatonin: (Major) Use caution when combining melatonin with other traditional sedatives and hypnotics, including the sedative barbiturates. Use of more than one agent for hypnotic purposes may increase the risk for over-sedation, CNS effects, or sleep-related behaviors. If a barbiturate is taken for seizure control, watch for changes in anticonvulsant activity. Be alert for unusual changes in moods or behaviors. Patients reporting unusual sleep-related behaviors likely should discontinue melatonin use. Additionally, melatonin exposure and efficacy may be reduced when combined with barbiturates such as phenobarbital, as barbiturates induce many CYP450 isoenzymes, including CYP1A2, the primary metabolic pathway for melatonin. (Minor) Caffeine is a central nervous system (CNS) stimulant. Patients taking melatonin for sleep should avoid caffeine-containing medications, dietary supplements, foods, and beverages close to bedtime, as well as excessive total daily caffeine intake, as part of proper sleep hygiene, since caffeine intake can interfere with proper sleep.
Meperidine: (Major) Concomitant use of meperidine with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concurrent use of meperidine with a barbiturate may decrease meperidine plasma concentrations, decrease opioid efficacy, and potentially lead to a withdrawal syndrome in those with physical dependence to opioid agonists. Monitor for signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of increased opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; meperidine is a CYP3A4 substrate.
Meperidine; Promethazine: (Major) Concomitant use of meperidine with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concurrent use of meperidine with a barbiturate may decrease meperidine plasma concentrations, decrease opioid efficacy, and potentially lead to a withdrawal syndrome in those with physical dependence to opioid agonists. Monitor for signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of increased opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; meperidine is a CYP3A4 substrate.
Mephobarbital: (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Mepivacaine: (Moderate) Coadministration of mepivacaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue mepivacaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
Mepivacaine; Levonordefrin: (Moderate) Coadministration of mepivacaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue mepivacaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
Meprobamate: (Major) Additive CNS depression may occur if barbiturates are used concomitantly with other anxiolytics, sedatives, and hypnotics like meprobamate. Caution should be exercised during concomitant use of anxiolytics, sedatives, and hypnotics and any barbiturate; dosage reduction of one or both agents may be necessary.
Mestranol; Norethindrone: (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol or combined hormonal oral contraceptives. This interaction occurs from the inhibition of methylxanthine oxidation in the liver. Patients may need to be informed about increased caffeine side effects, like nausea or tremors.
Metaproterenol: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Metformin; Repaglinide: (Major) Coadministration of barbiturates and repaglinide may decrease the serum concentration of repaglinide; if coadministration is necessary, a dose increase of repaglinide may be necessary and increased frequency of blood glucose monitoring. Barbiturates are CYP3A4 inducers and repaglinide is a CYP3A4 substrate. Monitor for the possibility of reduced effectiveness of repaglinide and possible symptoms indicating hyperglycemia.
Methadone: (Major) Concomitant use of methadone with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concurrent use of methadone with a barbiturate may decrease methadone plasma concentrations, decrease opioid efficacy, and potentially lead to a withdrawal syndrome in those with physical dependence to opioid agonists. Monitor for signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of increased opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates are inducers of CYP3A4, CYP2C9, and CYP2C19, isoenzymes partially responsible for the metabolism of methadone.
Methamphetamine: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants. Avoid excessive caffeine intake during use of methamphetamine. Excessive caffeine ingestion (via medicines, foods like chocolate, dietary supplements, or beverages including coffee, green tea, other teas, colas) may contribute to side effects like nervousness, irritability, nausea, insomnia, or tremor. Patients should avoid medications and dietary supplements which contain high amounts of caffeine.
Methazolamide: (Minor) Methazolamide can induce osteomalacia in patients treated chronically with barbiturates. Potential mechanisms for this interaction include a carbonic anhydrase inhibitor induced increase in the urinary excretion of calcium and an increase in barbiturate effects resulting from metabolic acidosis. Methazolamide can also increase the rate of excretion of weakly acidic drugs, such as barbiturates.
Methocarbamol: (Moderate) Methocarbamol may cause additive CNS depression if used concomitantly with other CNS depressants such as barbiturates. Dosage reduction of one or both agents may be necessary.
Methohexital: (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Methscopolamine: (Moderate) CNS depression can be increased when methscopolamine is combined with other CNS depressants such as any anxiolytics, sedatives, and hypnotics.
Methsuximide: (Moderate) Barbiturates induce hepatic microsomal enzymes and may increase the hepatic metabolism of succinimides. This may lead to a decrease in succinimide plasma concentration and a reduction in half-life.
Methyclothiazide: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Methylphenidate: (Moderate) Caffeine is a CNS stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants. Avoid excessive caffeine intake during use of methylphenidate. Excessive caffeine ingestion (via medicines, foods like chocolate, dietary supplements, or beverages including coffee, green tea, other teas, colas) may contribute to side effects like nervousness, irritability, nausea, insomnia, or tremor. Patients should avoid medications and dietary supplements which contain high amounts of caffeine.
Methylprednisolone: (Moderate) Coadministration may result in decreased exposure to methylprednisolone. Butalbital is a CYP3A4 inducer; methylprednisolone is a CYP3A4 substrate. Monitor for decreased response to methylprednisolone during concurrent use.
Metoclopramide: (Minor) Combined use of metoclopramide and other CNS depressants, such as anxiolytics, sedatives, and hypnotics, can increase possible sedation.
Metolazone: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Metronidazole: (Minor) Barbiturates may decrease the half-life and plasma concentrations of metronidazole. The clinical significance of this effect is uncertain.
Metyrapone: (Major) Coadministration of metyrapone and acetaminophen may result in acetaminophen toxicity. Acetaminophen glucuronidation is inhibited by metyrapone. It may be advisable for patients to avoid acetaminophen while taking metyrapone. (Moderate) Metyrapone may cause dizziness and/or drowsiness. Other drugs that may also cause drowsiness, such as barbiturates, should be used with caution. Additive drowsiness and/or dizziness is possible.
Metyrosine: (Moderate) The concomitant administration of metyrosine with barbiturates can result in additive sedative effects.
Mexiletine: (Moderate) Mexiletine is an inhibitor of CYP1A2 isoenzymes, and may reduce CYP1A2-mediated caffeine metabolism. Mexiletine has been shown to increase caffeine concentrations by as much as 23 percent after a single 200 mg dose of mexiletine (nonsignificant increase, p<0.1). Another study has reported that the elimination of caffeine is decreased by 50 percent. While the clinical significance of this interaction is not known, elevated plasma caffeine levels may be of concern in patients with arrhythmias. Patients with cardiac arrhythmias on mexiletine should be cautioned to limit their intake of caffeine. (Moderate) While other hepatic enzyme inducers have been shown to accelerate the metabolism of mexiletine, no data are available regarding the effects of barbiturates on mexiletine. An interaction between barbiturates and mexiletine, however, may be possible.
Midazolam: (Moderate) Additive CNS and/or respiratory depression may occur. Additionally, barbiturates may increase the metabolism of midazolam. Midazolam is a CYP3A4 substrate. Barbiturates are CYP3A4 inducers.
Midodrine: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants.
Minocycline: (Minor) Injectable minocycline contains magnesium sulfate heptahydrate. Because of the CNS-depressant effects of magnesium sulfate, additive central-depressant effects can occur following concurrent administration with CNS depressants such as barbiturates. Caution should be exercised when using these agents concurrently.
Mipomersen: (Moderate) Caution should be exercised when mipomersen is used with other medications known to have potential for hepatotoxicity, such as acetaminophen (> 4 g/day for >= 3 days/week). The effect of concomitant administration of mipomersen with other hepatotoxic medications is unknown. More frequent monitoring of liver-related tests may be warranted.
Mirtazapine: (Major) Monitor for excessive sedation and somnolence during coadministration of mirtazapine and barbiturates. Concurrent use may result in additive CNS depression.
Mitotane: (Moderate) Mitotane can cause sedation, lethargy, vertigo, and other CNS side effects. Concomitant administration of mitotane and CNS depressants may cause additive CNS effects. Mitotane should be used cautiously with other drugs that may cause CNS depression including barbiturates. (Minor) Use caution if mitotane and acetaminophen are used concomitantly, and monitor for decreased efficacy of acetaminophen. Mitotane is a strong CYP3A4 inducer and acetaminophen is a minor (10% to 15%) CYP3A4 substrate; coadministration may result in decreased plasma concentrations of acetaminophen.
Modafinil: (Major) It is not clear how modafinil interacts with barbiturates like phenobarbital. Modafinil is partially metabolized by CYP3A4 and combined use with CYP3A4 inducers such as phenobarbital and other barbiturates may result in decreased modafinil efficacy. Barbiturates used for sleep could counteract the effect of modafinil on wakefulness, and would not ordinarily be prescribed. The potential effects of combining modafinil with anticonvulsant barbiturate medications are unclear. Many psychostimulants can reduce the seizure threshold, but it is not clear if modafinil can affect seizure control. (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants. Caffeine should be used cautiously with modafinil. Excessive intake should be limited. Excessive intake may cause nervousness, irritability, insomnia or other side effects.
Monoamine oxidase inhibitors: (Major) Additive CNS depression may occur if butalbital is used concomitantly with monoamine oxidase inhibitors. (Major) Excessive use of caffeine in any form should be avoided in patients receiving Monoamine oxidase inhibitors (MAOIs). Limit caffeine intake during MAOI use and for 1 to 2 weeks after discontinuation of any MAOI. the use of non-prescription medicines or dietary supplements containing caffeine should be avoided. Patients should try to avoid or limit the intake of all items containing caffeine such as tea, coffee, chocolate, and cola. Cardiac arrhythmias or severe hypertension may occur because of the potentiation of caffeine’s sympathomimetic effects by MAOIs if caffeine intake is excessive. Ordinarily, selegiline may be an exception, it can only be used safely without dietary restrictions at doses where it presumably selectively inhibits MAO-B (e.g., 10 mg/day). At doses of 20 mg/day, selegiline can interact with foods and beverages. The precise dose at which selegiline becomes a non-selective inhibitor of all MAO is unknown, but may be in the range of 30 to 40 mg per day. Attention to the dose dependent nature of selegiline’s selectivity is critical if it is to be used without elaborate restrictions being placed on diet.
Morphine: (Major) Concomitant use of morphine with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. For extended-release morphine tablets (MS Contin and Morphabond), start with 15 mg every 12 hours. Morphine; naltrexone should be initiated at 1/3 to 1/2 the recommended starting dosage. Educate patients about the risks and symptoms of respiratory depression and sedation.
Morphine; Naltrexone: (Major) Concomitant use of morphine with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. For extended-release morphine tablets (MS Contin and Morphabond), start with 15 mg every 12 hours. Morphine; naltrexone should be initiated at 1/3 to 1/2 the recommended starting dosage. Educate patients about the risks and symptoms of respiratory depression and sedation.
Nabilone: (Moderate) Concomitant use of nabilone with other CNS depressants, like barbiturates, can potentiate the effects of nabilone on respiratory depression.
Nalbuphine: (Moderate) Additive CNS depression may occur if barbiturates are used concomitantly with nalbuphine. Caution should be exercised during concomitant use of nalbuphine and any barbiturate. Dosage reduction of one or both agents may be necessary.
Naproxen; Pseudoephedrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Nelfinavir: (Major) Coadministration with phenobarbital and, potentially, other barbiturates may increase the metabolism of nelfinavir and lead to decreased nelfinavir concentrations resulting in reduction of antiretroviral efficacy and development of viral resistance. If nelfinavir and barbiturates are used together, the patient must be closely monitored for antiviral efficacy.
Neratinib: (Major) Avoid concomitant use of butalbital with neratinib due to decreased efficacy of neratinib. Neratinib is a CYP3A4 substrate and butalbital is a moderate CYP3A4 inducer. The effect of moderate CYP3A4 induction on neratinib concentrations has not been studied; however, coadministration with a strong CYP3A4 inducer decreased neratinib exposure by 87% and decreased exposure to active metabolites M6 and M7 by 37% to 49%. Because of the significant impact on neratinib exposure from strong CYP3A4 induction, the potential impact on neratinib efficacy from concomitant use with moderate CYP3A4 inducers should be considered as they may also significantly decrease neratinib exposure.
Nevirapine: (Moderate) Coadministration of nevirapine with barbiturates, which induce the activity of CYP3A, would be expected to increase the clearance of nevirapine, thereby decreasing nevirapine plasma concentrations. However, since nevirapine also induces CYP3A enzymes, decreases in anticonvulsant serum concentrations may be noted with the possibility of new seizure activity. The appropriate drug-dose adjustments necessary to ensure optimum levels of both antiretroviral drugs and barbiturates are unknown. If used concomitantly, the patient should be observed for changes in the clinical efficacy and concentrations of the antiretroviral and anticonvulsant regimens.
Niacin; Simvastatin: (Moderate) Barbiturates are significant hepatic CYP3A4 inducers. Monitor for potential reduced cholesterol-lowering efficacy when barbiturates are co-administered with simvastatin, which is metabolized by CYP3A4.
Nicardipine: (Major) Patients should be monitored for loss of antihypertensive effect if CYP3A4 enzyme inducers like the barbiturates are added to nicardipine therapy. Rifampin is a potent hepatic enzyme inducer and has been shown to exert a substantial reduction of the oral bioavailability of some calcium channel blockers. This interaction should be considered with other potent CYP3A4 inhibitors including the barbiturates.
Nifedipine: (Major) Avoid coadministration of nifedipine with barbiturates and consider alternative therapy if possible. If coadministration is necessary, monitor the patient closely for desired cardiovascular effects on heart rate, blood pressure, or chest pain. The FDA-approved labeling for some nifedipine products contraindicates coadministration with strong CYP3A4 inducers, while other manufacturers classify the recommendation as a warning. Nifedipine is a CYP3A4 substrate, and barbiturates are strong CYP3A4 inducers. Coadministration of nifedipine with another strong CYP3A4 inducer reduced the AUC and Cmax of nifedipine by approximately 70%.
Nimodipine: (Major) In epileptic patients taking phenobarbital with or without other enzyme-inducing anticonvulsants, there is a 7-fold decrease in the AUC of nimodipine due to hepatic enzyme induction. Patients receiving barbiturates and nimodipine concomitantly should be monitored closely for efficacy. Although no data are available, it is likely that nimodipine, a CYP3A4 substrate, may be affected by the coadministration of all barbiturates.
Nintedanib: (Major) Avoid the use of barbiturates with nintedanib, as these drugs are expected to decrease the exposure of nintedanib and compromise its efficacy. Barbiturates are CYP3A4 inducers and some barbiturates, such as phenobarbital, also induce P-glycoprotein (P-gp). In drug interaction studies, administration of a dual P-gp and CYP3A4 inducer with nintedanib decreased the AUC of nintedanib by 50%.
Nisoldipine: (Major) Coadministration of nisoldipine with CYP3A4 inducers like the barbiturates should be avoided and alternative antihypertensive therapy should be considered. Coadministration of a strong CYP3A4 inducer with nisoldipine in epileptic patients lowered the nisoldipine plasma concentrations to undetectable levels. Barbiturates (e.g., phenobarbital, primidone) may also decrease the oral bioavailability of nisoldipine via increased hepatic drug clearance.
Non-Ionic Contrast Media: (Major) Use of medications that lower the seizure threshold should be carefully evaluated when considering intrathecal radiopaque contrast agents. Caffeine and caffeine containing products should be discontinued at least 48 hours before myelography and should not be resumed for at least 24 hours post-procedure.
Norepinephrine: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants.
Obeticholic Acid: (Moderate) Obeticholic acid may increase the exposure to concomitant drugs that are CYP1A2 substrates, such as caffeine. Concomitant administration of 200 mg caffeine as a single dose with obeticholic acid 10 mg once daily resulted in a 42% increase in caffeine AUC and a 6% increase in caffeine Cmax. Therapeutic monitoring is recommended with coadministration. No specific management is recommended except in patients who complain of caffeine-related side effects like nausea, tremor, or palpitations. In such patients, the dosage of caffeine-containing medications or the ingestion of caffeine-containing products may need to be reduced.
Olanzapine: (Moderate) Olanzapine is metabolized by the CYP1A2 hepatic microsomal isoenzyme, and inducers of this enzyme such as barbiturates, may increase olanzapine clearance. The clinical effect of this interaction is thought to be minimal; however, the clinician should be alert for reduced olanzapine effect if the drugs are coadministered. Additive effects are possible when olanzapine is combined with other drugs which cause respiratory depression and/or CNS depression. Barbiturates can cause CNS depression, and if used concomitantly with olanzapine, can increase both the frequency and the intensity of adverse effects such as drowsiness, sedation, dizziness, and orthostatic hypotension.
Olaparib: (Major) Avoid the coadministration of olaparib with butalbital due to decreased olaparib exposure; if concomitant use is unavoidable, there is a potential for decreased efficacy of olaparib. Olaparib is a CYP3A4 substrate and butalbital is a moderate CYP3A4 inducer. Coadministration with a moderate CYP3A inducer is predicted to decrease the AUC of olaparib by 60%.
Olodaterol: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Ombitasvir; Paritaprevir; Ritonavir: (Major) Concurrent use of ritonavir with phenobarbital or other barbiturates should be done cautiously. Increased doses of anticonvulsants may be required due metabolism induction by ritonavir. However, since these anticonvulsants are hepatic enzyme inducing drugs, increased metabolism of protease inhibitors may occur, leading to decreased antiretroviral efficacy. Close monitoring of drug concentrations and/or therapeutic and adverse effects is required. (Moderate) Concurrent administration of acetaminophen with ritonavir may result in elevated acetaminophen plasma concentrations and subsequent adverse events. Acetaminophen is metabolized by the hepatic isoenzyme CYP3A4; ritonavir is an inhibitor of this enzyme. Caution and close monitoring are advised if these drugs are administered together.
Omeprazole: (Major) Avoid coadministration of omeprazole with barbiturates because it can result in decreased efficacy of omeprazole. Omeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19.
Omeprazole; Sodium Bicarbonate: (Major) Avoid coadministration of omeprazole with barbiturates because it can result in decreased efficacy of omeprazole. Omeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. (Minor) Antacids can delay the oral absorption of acetaminophen, but the interactions are not likely to be clinically significant as the extent of acetaminophen absorption is not appreciably affected.
Ondansetron: (Minor) Ondansetron elimination may be affected by cytochrome P-450 inducers. In a pharmacokinetic study of 16 patients with epilepsy who were maintained chronically on CYP3A4 inducers (e.g., barbiturates) a reduction in ondansetron AUC, Cmax, and half-life was observed, resulting in a significant increase in ondansetron clearance. However, these changes in ondansetron exposure are not thought to be clinically relevant; no dosage adjustment for ondansetron is recommended when CYP450 inducers are used concurrently.
Oxazepam: (Moderate) Additive CNS and/or respiratory depression may occur with concurrent use.
Oxybutynin: (Moderate) Additive CNS depression may occur when oxybutynin is used concomitantly with other CNS-depressant drugs, including anxiolytics, sedatives, and hypnotics. In addition, because oxybutynin is metabolized by CYP3A4, administration with drugs that induce CYP3A4 (such as barbiturates) may reduce the serum concentration and effects of oxybutynin. Patients receiving these drugs concomitantly should be monitored for reduced efficacy. (Minor) Consuming greater than 400 mg/day caffeine has been associated with the development of urinary incontinence. Caffeine may aggravate bladder symptoms, increase urine output, and counteract the effectiveness of drugs used to treat overactive bladder such as oxybutynin. Patients may wish to limit their intake of caffeinated drugs, dietary supplements (e.g., guarana), or beverages (e.g., green tea, other teas, coffee, colas).
Oxycodone: (Major) Concomitant use of oxycodone with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concurrent use of oxycodone with a barbiturate may decrease oxycodone plasma concentrations, decrease opioid efficacy, and potentially lead to a withdrawal syndrome in those with physical dependence to opioid agonists. Monitor for signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of increased opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; oxycodone is a CYP3A4 substrate.
Oxymorphone: (Major) Concomitant use of oxymorphone with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Reduce the initial oxymorphone dosage by 1/3 to 1/2. Educate patients about the risks and symptoms of respiratory depression and sedation.
Paclitaxel: (Minor) Paclitaxel is metabolized by hepatic cytochrome P450 isoenzymes 2C8 and 3A4. Potential interactions may occur in vivo with any agent that induces CYP2C8 or CYP3A4 isoenzymes including barbiturates.
Paliperidone: (Major) Avoid using a strong inducer of CYP3A4 if possible during the 1-month injectable dosing interval of Invega Sustenna or the 3-month injectable dosing interval of Invega Trinza. If use of a strong CYP3A4 inducer such as a barbiturate is required in patients receiving injectable paliperidone, consider management with oral paliperidone. Paliperidone is a P-gp substrate, with minor contributions in metabolism by CYP3A4 and CYP2D6. A dosage increase of oral paliperidone may be required during coadministration of a strong inducer of both CYP3A4 and P-gp. However, concurrent use of oral paliperidone with a strong CYP3A4 inducer alone may not be clinically relevant since this isoenzyme contributes to only a small fraction of total body clearance of the drug. It should be noted that clinically significant barbiturate enzyme-induction occurs after several days and may not be clinically significant with short-term use of barbiturates.
Papaverine: (Moderate) Concurrent use of papaverine with potent CNS depressants such as barbiturates could lead to enhanced sedation.
Paroxetine: (Moderate) Barbiturates may induce various hepatic CYP450 isoenzymes, including those responsible for the metabolism of paroxetine. Clinicians should be aware of the potential for reduced SSRI efficacy with concurrent administration of a barbiturate, especially in chronic use.
Peginterferon Alfa-2b: (Moderate) The effects of peginterferon alfa-2b on CYP1A2 were evaluated in drug interaction studies. Administration of peginterferon alfa-2b with caffeine, a CYP1A2 substrate, resulted in an 18% to 39% increase in the geographic mean exposure for caffeine, suggesting inhibition of CYP1A2. Monitor for adverse effects associated with increased exposure to caffeine if peginterferon alfa-2b is coadministered with caffeine.
Pemoline: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants.
Penicillin G Benzathine; Penicillin G Procaine: (Moderate) Coadministration of penicillin G procaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue penicillin G procaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
Penicillin G Procaine: (Moderate) Coadministration of penicillin G procaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue penicillin G procaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
Pentazocine: (Moderate) Concomitant use of pentazocine with other CNS depressants can potentiate respiratory depression, CNS depression, and sedation. Pentazocine should be used cautiously in any patient receiving these agents, which may include barbiturates.
Pentazocine; Naloxone: (Moderate) Concomitant use of pentazocine with other CNS depressants can potentiate respiratory depression, CNS depression, and sedation. Pentazocine should be used cautiously in any patient receiving these agents, which may include barbiturates.
Pentobarbital: (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Perampanel: (Moderate) Co-administration of perampanel with CNS depressants, including ethanol, may increase CNS depression. The combination of perampanel (particularly at high doses) with ethanol has led to decreased mental alertness and ability to perform complex tasks (such as driving), as well as increased levels of anger, confusion, and depression; similar reactions should be expected with concomitant use of other CNS depressants, such as barbiturates.
Perindopril; Amlodipine: (Major) Barbiturates may induce the CYP3A4 metabolism of calcium-channel blockers such as amlodipine, and thereby reduce their oral bioavailability. The dosage requirements of amlodipine may be increased in patients receiving concurrent enzyme inducers; monitor blood pressure closely.
Phendimetrazine: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants.
Phenelzine: (Major) Additive CNS depression may occur if butalbital is used concomitantly with monoamine oxidase inhibitors. (Major) Excessive use of caffeine in any form should be avoided in patients receiving Monoamine oxidase inhibitors (MAOIs). Limit caffeine intake during MAOI use and for 1 to 2 weeks after discontinuation of any MAOI. the use of non-prescription medicines or dietary supplements containing caffeine should be avoided. Patients should try to avoid or limit the intake of all items containing caffeine such as tea, coffee, chocolate, and cola. Cardiac arrhythmias or severe hypertension may occur because of the potentiation of caffeine’s sympathomimetic effects by MAOIs if caffeine intake is excessive. Ordinarily, selegiline may be an exception, it can only be used safely without dietary restrictions at doses where it presumably selectively inhibits MAO-B (e.g., 10 mg/day). At doses of 20 mg/day, selegiline can interact with foods and beverages. The precise dose at which selegiline becomes a non-selective inhibitor of all MAO is unknown, but may be in the range of 30 to 40 mg per day. Attention to the dose dependent nature of selegiline’s selectivity is critical if it is to be used without elaborate restrictions being placed on diet.
Phenobarbital: (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Phenothiazines: (Moderate) Phenothiazines are CNS depressant drugs that may have cumulative effects when administered concurrently and they should be used cautiously with anxiolytic, sedative, and hypnotic type drugs, such as the barbiturates. Caution should be exercised during simultaneous use of these agents due to potential excessive CNS effects or additive hypotension. Phenothiazines can also lower the seizure threshold, which may be important in patients taking a barbiturate for the treatment of seizures. Additionally, sleep-related behaviors, such as sleep-driving, are more likely to occur during concurrent use of other CNS depressants than with the use of sedatives alone. Monitor for additive effects, unusual moods or behaviors, and warn about the potential effects to driving and other activities.
Phentermine: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants.
Phentermine; Topiramate: (Moderate) Although topiramate is not extensively metabolized (70% renally eliminated), an interaction with barbiturates via hepatic isoenzyme activity is possible. In patients receiving either phenobarbital or primidone in combination with topiramate, there was a < 10% change in phenobarbital or primidone plasma concentrations; the effects on topiramate plasma concentrations were not evaluated. Barbiturates may cause additive sedation or other CNS depressive effects when used concurrently with topiramate. When topiramate is combined with phentermine for the treatment of obesity, a greater risk of CNS depression exists. Concurrent use of topiramate and drugs that cause thrombocytopenia, such as the barbiturates, may also increase the risk of bleeding; monitor patients appropriately. (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants.
Phenylephrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Phenylephrine; Promethazine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants like phenylephrine; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Pimavanserin: (Major) Because pimavanserin is primarily metabolized by CYP3A4 and CYP3A5, the manufacturer recommends avoiding concomitant use of pimavanserin with strong CYP3A4 inducers, such as barbiturates. Strong inducers of CYP3A4 reduce pimavanserin exposure, potentially decreasing the effectiveness of pimavanserin.
Pirbuterol: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Pneumococcal Vaccine, Polyvalent: (Moderate) Concomitant administration of antipyretics, such as acetaminophen, may decrease an individual’s immunological response to the pneumococcal vaccine. A post-marketing study conducted in Poland using a non-US vaccination schedule (2, 3, 4, and 12 months of age) evaluated the impact of prophylactic oral acetaminophen on antibody responses to Prevnar 13. Data show that acetaminophen, given at the time of vaccination and then dosed at 6 to 8 hour intervals for 3 doses on a scheduled basis, reduced the antibody response to some serotypes after the third dose of Prevnar 13 when compared to the antibody responses of infants who only received antipyretics ‘as needed’ for treatment. However, reduced antibody responses were not observed after the fourth dose of Prevnar 13 with prophylactic acetaminophen.
Pomalidomide: (Moderate) Use pomalidomide and barbiturates together with caution; decreased pomalidomide exposure may occur resulting in reduced pomalidomide effectiveness. Pomalidomide is a CYP1A2 substrate and barbiturates are CYP1A2 inducers.
Posaconazole: (Moderate) Posaconazole and acetaminophen should be coadministered with caution due to an increased potential for acetaminophen-related adverse events. Posaconazole is a potent inhibitor of CYP3A4, an isoenzyme partially responsible for the metabolism of acetaminophen. These drugs used in combination may result in elevated acetaminophen plasma concentrations, causing an increased risk for acetaminophen-related adverse events.
Pralidoxime: (Major) The action of barbiturates is potentiated by the acetylcholinesterase inhibitors, which should be considered when using pralidoxime. Barbiturates should be used with caution to treat convulsions produced by acetylcholinesterase inhibitors.
Pramipexole: (Major) The use of barbiturates in combination with pramipexole may increase the risk of clinically significant sedation via a pharmacodynamic interaction.
Pramlintide: (Minor) Because pramlintide has the potential to delay the absorption of concomitantly administered medications, medications should be administered at least 1 hour before or 2 hours after pramlintide injection when the rapid onset of a concomitantly administered oral medication is a critical determinant of effectiveness (i.e., analgesics).
Prednisolone: (Moderate) Coadministration may result in decreased exposure to prednisolone. Butalbital is a CYP3A4 inducer; prednisolone is a CYP3A4 substrate. Monitor for decreased response to prednisolone during concurrent use.
Prednisone: (Moderate) Coadministration may result in decreased exposure to prednisone. Butalbital is a CYP3A4 inducer; prednisone is a CYP3A4 substrate. Monitor for decreased response to prednisone during concurrent use.
Pregabalin: (Moderate) Concomitant administration of pregabalin with CNS-depressant drugs, including barbiturates, can potentiate the CNS effects of either agent. Pregabalin can cause considerable somnolence and the combined use of ethanol or other CNS depressants with pregabalin may lead to an additive drowsy effect.
Prilocaine: (Moderate) Coadministration of prilocaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue prilocaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
Prilocaine; Epinephrine: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants. (Moderate) Coadministration of prilocaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue prilocaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
Primidone: (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Procarbazine: (Major) Ingestion of certain products should be minimized while receiving procarbazine therapy, as the drug has some MAO inhibiting actions. Caffeine may produce hypertension or hypertensive crisis or induce cardiac arrhythmias if administered to patients taking drugs with strong MAOI properties. All preparations containing caffeine should be used sparingly such as teas, coffee, chocolate, cola, guarana, or ‘stay awake’ products. Some non-prescription medicines also contain caffeine and should not be taken without health care professional advice. Following discontinuation of procarbazine, dietary restrictions should continue for at least 2 weeks due to the slow recovery from the enzyme-inhibiting effects. (Moderate) Use procarbazine and barbiturates together with caution; additive CNS depression may occur.
Progestins: (Moderate) Barbiturates can accelerate the hepatic clearance of progestins. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. The exception is the use of levonorgestrel progestin IUDs, which have not been reported to interact and appear to maintain reliable efficacy. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking progestins for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment.
Pseudoephedrine: (Moderate) CNS-stimulating actions of caffeine can be additive with other CNS stimulants or psychostimulants; caffeine should be avoided or used cautiously. Excessive caffeine ingestion (via medicines, supplements or beverages including coffee, green tea, other teas, guarana, colas) may contribute to side effects like nervousness, irritability, insomnia, or tremor.
Quazepam: (Moderate) Additive CNS and/or respiratory depression may occur. Additionally, barbiturates may increase the metabolism of quazepam. Quazepam is a CYP2C9, CYP2C19, and CYP3A4 substrate. Barbiturates are CYP2C9, CYP2C19, and CYP3A4 inducers.
Quetiapine: (Major) Coadministration of barbiturates, potent CYP3A4 inducers, with quetiapine, a CYP3A4 substrate, may result in decreased exposure to quetiapine. The dose of quetiapine should be increased by up to 5-fold when combined with chronic administration (7 to 14 days) of a potent CYP3A4 inducer. Adjust the dose based on patient response and tolerability. When the potent CYP3A4 inducer is discontinued, the quetiapine dose should be reduced to the original dose within 1 to 2 weeks. Also, somnolence is a commonly reported adverse effect of quetiapine; coadministration of quetiapine with barbiturates may result in additive sedative effects.
Quinidine: (Major) Quinidine is eliminated primarily via hepatic metabolism, primarily by the CYP3A4 isoenzyme. Administration of other hepatic enzyme inducers, such as barbiturates, can accelerate quinidine elimination and decrease its serum concentrations. Phenobarbital may decrease quinidine half-life and corresponding AUC by about 50 to 60%. Quinidine concentrations should be monitored closely after one of these agents is added. No special precautions appear necessary if these agents are begun several weeks before quinidine is added but quinidine doses may require adjustment if one of these agents is added or discontinued during quinidine therapy.
Quinine: (Major) If concomitant administration of barbiturates and quinine cannot be avoided, frequently monitor the barbiturate concentration. Also, monitor closely for increased barbiturate-associated adverse events such as excessive drowsiness, difficulty breathing, or confusion. A single quinine 600 mg dose increased the mean plasma Cmax and AUC of a barbiturate by 53% and 81%, respectively, in 8 healthy subjects. In addition, barbiturates are CYP3A4 inducers and may decrease plasma quinine concentrations.
Rabeprazole: (Moderate) Concurrent administration of rabeprazole with barbiturates may result in decreased rabeprazole plasma concentrations; monitor for signs and symptoms of reduced rabeprazole efficacy. Barbiturates induce CYP2C19 and rabeprazole is a CYP2C19 substrate.
Racepinephrine: (Moderate) Patients who are using racepinephrine inhalation are advised to avoid foods and beverages that contain caffeine. They should also avoid dietary supplements containing ingredients, such as caffeine, that are reported or claimed to have a stimulant effect. If a patient is taking prescribed medications containing caffeine, then they should seek health care professional advice prior to the use of racepinephrine. Additive adverse effects on the cardiovascular and nervous system are possible, some which may be undesirable. Side effects such as nausea, tremor, nervousness, difficulty with sleep, and increased heart rate may be additive. Consider alternatives to racepinephrine for the treatment of asthma.
Ramelteon: (Major) Barbiturates can induce CYP1A2, the major metabolic pathway for ramelteon, and may eventually accelerate the clearance (and, thus, reduce the sedative properties) of ramelteon. Administration of multiple doses of a potent CYP inducer (rifampin) resulted in a mean decrease of approximately 80% in total exposure to ramelteon and its metabolite M-II. Additive CNS depression may also occur. The induction of ramelteon metabolism would likely require several days of barbiturate administration while additive drowsiness would appear immediately. Caution should be exercised during concomitant use of any CNS-depressant drugs and any barbiturate; dosage reduction of one or both agents may be necessary. If the medications must be used together, monitor for the effectiveness of ramelteon. Hypnotic barbiturates are best avoided during ramelteon therapy; the manufacturer warns against using other medications for sleep concurrently with ramelteon. (Minor) Caffeine is a central nervous system (CNS) stimulant. Patients taking melatonin or the melatonin analogs (ramelteon, tasimelteon) for sleep should avoid caffeine-containing medications, dietary supplements, foods, and beverages close to bedtime. Patients should be encouraged to avoid excessive total daily caffeine intake, as part of proper sleep hygiene, since caffeine intake can interfere with proper sleep.
Ranolazine: (Severe) Ranolazine is contraindicated in patients receiving drugs known to be CYP3A inducers including barbiturates. Induction of CYP3A metabolism could lead to decreased ranolazine plasma concentrations and decreased efficacy.
Rasagiline: (Moderate) Although sympathomimetics and psychostimulants are contraindicated for use with other monoamine oxidase inhibitors (MAOIs), hypertensive reactions generally are not expected to occur during concurrent use with rasagiline because of the selective monoamine oxidase-B (MAO-B) inhibition of rasagiline at manufacturer recommended doses. (Moderate) The CNS-depressant effects of MAOIs can be potentiated with concomitant administration of other drugs known to cause CNS depression including buprenorphine, butorphanol, dronabinol, THC, nabilone, nalbuphine, and anxiolytics, sedatives, and hypnotics. Use these drugs cautiously with MAOIs; warn patients to not drive or perform other hazardous activities until they know how a particular drug combination affects them. In some cases, the dosages of the CNS depressants may need to be reduced.
Red Yeast Rice: (Moderate) Since certain red yeast rice products (i.e., pre-2005 Cholestin formulations) contain lovastatin, clinicians should use red yeast rice cautiously in combination with drugs known to interact with lovastatin. CYP3A4 inducers, such as barbiturates, can theoretically reduce the effectiveness of HMG-CoA reductase activity via induction of CYP3A4 metabolism.
Regadenoson: (Major) Caffeine is a non-specific adenosine receptor antagonist and can interfere with the efficacy of regadenoson. Patients should avoid consumption of any products containing caffeine (including caffeine from foods and beverages such as coffee, green tea, other teas, colas, and chocolate) for at least 12 hours before regadenoson administration.
Remifentanil: (Major) Concomitant use of remifentanil with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation.
Repaglinide: (Major) Coadministration of barbiturates and repaglinide may decrease the serum concentration of repaglinide; if coadministration is necessary, a dose increase of repaglinide may be necessary and increased frequency of blood glucose monitoring. Barbiturates are CYP3A4 inducers and repaglinide is a CYP3A4 substrate. Monitor for the possibility of reduced effectiveness of repaglinide and possible symptoms indicating hyperglycemia.
Reserpine: (Moderate) Administration of reserpine can potentiate the depressant effects of CNS depressants such as barbiturates.
Rifabutin: (Moderate) As a cytochrome P450 isoenzyme inducers, rifabutin could induce the metabolism of acetaminophen. An increase in acetaminophen-induced hepatotoxicity may be seen by increasing the metabolism of acetaminophen to its toxic metabolite, NAPQI. Also, the analgesic activity of acetaminophen may be reduced.
Rifampin: (Moderate) Agents which induce the hepatic isoenzymes CYP2E1 and CYP1A2, such as rifampin, may potentially increase the risk for acetaminophen-induced hepatotoxicity via generation of a greater percentage of acetaminophen’s hepatotoxic metabolites. (Moderate) It may be necessary to adjust the dosage of butalbital if given concurrently with rifampin. Rifampin may induce the metabolism of butalbital; coadministration may result in decreased butalbital plasma concentrations. (Minor) Rifampin is a potent inducer of the cytochrome P450 hepatic enzyme system and can reduce the plasma concentrations and possibly the efficacy of caffeine, including caffeine found in green tea products.
Rifapentine: (Moderate) Rifapentine induces hepatic isoenzymes CYP3A4 and CYP2C8/9. Drugs metabolized by these enzymes, like barbiturates, may require dosage adjustments when administered concurrently with rifapentine.
Rilpivirine: (Moderate) Close clinical monitoring is advised when administering barbiturates with rilpivirine due to the potential for rilpivirine treatment failure. Although this interaction has not been studied, predictions can be made based on metabolic pathways. Barbiturates are inducers of the hepatic isoenzyme CYP3A4; rilpivirine is metabolized by this isoenzyme. Coadministration may result in decreased rilpivirine serum concentrations and impaired virologic response.
Riluzole: (Moderate) Coadministration of riluzole with barbiturates may result in decreased riluzole efficacy. In vitro findings suggest decreased riluzole exposure is likely. Riluzole is a CYP1A2 substrate and barbiturates are CYP1A2 inducers.
Risperidone: (Major) Potent inducers of CYP3A4, such as barbiturates, may decrease plasma concentrations of risperidone and its active metabolite. Therefore, the manufacturer of oral risperidone recommends a slow upward titration of the risperidone dose as needed up to double the patient’s usual dose during use of a 3A4 inducer. When using Risperdal Consta, the patient will require close monitoring for 4 to 8 weeks when starting an inducer. A lower dose of Risperdal Consta may be prescribed between 2 to 4 weeks before the planned discontinuation of the inducer to adjust for the expected increase in plasma concentrations of risperidone and its active metabolite. For patients treated with the recommended dose of Risperdal Consta 25 mg and discontinuing the inducer, it is recommended to continue the 25 mg dose unless a reduction to 12.5 mg or discontinuation of treatment is indicated. The efficacy of the 12.5 mg dose has not been studied in clinical trials.
Ritodrine: (Moderate) Caffeine is a CNS-stimulant and such actions are expected to be additive when coadministered with other CNS stimulants or psychostimulants.
Ritonavir: (Major) Concurrent use of ritonavir with phenobarbital or other barbiturates should be done cautiously. Increased doses of anticonvulsants may be required due metabolism induction by ritonavir. However, since these anticonvulsants are hepatic enzyme inducing drugs, increased metabolism of protease inhibitors may occur, leading to decreased antiretroviral efficacy. Close monitoring of drug concentrations and/or therapeutic and adverse effects is required. (Moderate) Concurrent administration of acetaminophen with ritonavir may result in elevated acetaminophen plasma concentrations and subsequent adverse events. Acetaminophen is metabolized by the hepatic isoenzyme CYP3A4; ritonavir is an inhibitor of this enzyme. Caution and close monitoring are advised if these drugs are administered together.
Roflumilast: (Major) Coadminister barbiturates and roflumilast cautiously as this may lead to reduced systemic exposure to roflumilast. Barbiturates induce CYP3A4 and roflumilast is a CYP3A4 substrate. In pharmacokinetic study, administration of a single dose of roflumilast in patients receiving another CYP3A4 inducer, rifampin, resulted in decreased roflumilast Cmax and AUC, as well as increased Cmax and decreased AUC of the active metabolite roflumilast N-oxide.
Romidepsin: (Moderate) Romidepsin is a substrate for CYP3A4. Coadministration of CYP3A4 inducers, like barbiturates, may decrease systemic concentrations of romidepsin. Use caution when concomitant administration of these agents is necessary.
Ropinirole: (Moderate) Coadministration of ropinirole and barbiturates may result in decreased concentrations of ropinirole. If therapy with barbiturates is initiated or discontinued during treatment with ropinirole, adjustment of ropinirole dose may be required. Ropinirole is primarily metabolized by CYP1A2; barbiturates are inducers of CYP1A2. Also, somnolence is a commonly reported adverse effect of ropinirole; coadministration of ropinirole with barbiturates may result in additive sedative effects.
Ropivacaine: (Moderate) Coadministration of ropivacaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue ropivacaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
Rotigotine: (Major) Concomitant use of rotigotine with other CNS depressants, such as butalbital, can potentiate the sedation effects of rotigotine.
Rucaparib: (Moderate) Monitor for an increase in caffeine-related adverse reactions if coadministration with rucaparib is necessary. Some patients may need to reduce or limit their caffeine intake. Caffeine is a sensitive CYP1A2 substrate and rucaparib is a weak CYP1A2 inhibitor. Concomitant use increased the AUC of caffeine by 2.55-fold.
Safinamide: (Moderate) Dopaminergic medications, including safinamide, may cause a sudden onset of somnolence which sometimes has resulted in motor vehicle accidents. Patients may not perceive warning signs, such as excessive drowsiness, or they may report feeling alert immediately prior to the event. Because of possible additive effects, advise patients about the potential for increased somnolence during concurrent use of safinamide with other sedating medications, such as barbiturates.
Salicylates: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur.
Salmeterol: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Salsalate: (Moderate) Due to high protein binding, salicylates could be displaced from binding sites, or could displace other highly protein-bound drugs such as barbiturates. An enhanced effect of the displaced drug may occur. (Moderate) Prolonged concurrent use of acetaminophen and salicylates is not recommended. Although salicylates are rarely associated with nephrotoxicity, high-dose, chronic administration of salicylates combined other analgesics, including acetaminophen, significantly increases the risk of analgesic nephropathy, renal papillary necrosis, and end-stage renal disease. Additive hepatic toxicity may occur, especially in combined overdose situations. Do not exceed the recommended individual maximum doses when these agents are given concurrently for short-term therapy.
Saquinavir: (Major) Coadministration with phenobarbital and, potentially, other barbiturates may increase the metabolism of saquinavir and lead to decreased saquinavir concentrations resulting in reduction of antiretroviral efficacy and development of viral resistance. If saquinavir and barbiturates are used together, the patient must be closely monitored for antiviral efficacy.
Scopolamine: (Moderate) Scopolamine may cause dizziness and drowsiness. Concurrent use of scopolamine and CNS depressants can adversely increase the risk of CNS depression.
Secobarbital: (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Segesterone Acetate; Ethinyl Estradiol: (Moderate) Acetaminophen may increase plasma ethinyl estradiol levels, possibly by inhibition of conjugation. Patients taking acetaminophen concomitantly may experience an increase in estrogen related side effects. (Moderate) Barbiturates can accelerate the hepatic clearance of estrogens. For hormonal contraceptives, this interaction could result in unintended pregnancy or breakthrough bleeding. For patients regularly taking a barbiturate, an alternative or back-up method of contraception may be advisable to ensure contraceptive reliability during the use of the barbiturate, and for 1 month following the discontinuation of barbiturate use. Pregnancy has been reported during therapy with both estrogen- and/or progestin-based oral contraceptives in patients receiving barbiturates (e.g., phenobarbital). For patients taking estrogens for other indications, like hormone replacement, monitor the patient for signs and symptoms of reduced therapeutic efficacy or need for dosage adjustment. (Minor) Serum concentrations of caffeine may be increased during concurrent administration with ethinyl estradiol. Patients may desire to limit products that contain high amounts of caffeine to minimize caffeine-related side effects such as nausea or tremors.
Selegiline: (Major) Additive CNS depression may occur if butalbital is used concomitantly with monoamine oxidase inhibitors. (Major) Excessive use of caffeine in any form should be avoided in patients receiving Monoamine oxidase inhibitors (MAOIs). Limit caffeine intake during MAOI use and for 1 to 2 weeks after discontinuation of any MAOI. the use of non-prescription medicines or dietary supplements containing caffeine should be avoided. Patients should try to avoid or limit the intake of all items containing caffeine such as tea, coffee, chocolate, and cola. Cardiac arrhythmias or severe hypertension may occur because of the potentiation of caffeine’s sympathomimetic effects by MAOIs if caffeine intake is excessive. Ordinarily, selegiline may be an exception, it can only be used safely without dietary restrictions at doses where it presumably selectively inhibits MAO-B (e.g., 10 mg/day). At doses of 20 mg/day, selegiline can interact with foods and beverages. The precise dose at which selegiline becomes a non-selective inhibitor of all MAO is unknown, but may be in the range of 30 to 40 mg per day. Attention to the dose dependent nature of selegiline’s selectivity is critical if it is to be used without elaborate restrictions being placed on diet.
Sertraline: (Moderate) Sertraline is a substrate for CYP3A4 and CYP2C19. Drugs that induce hepatic isoenzymes, such as barbiturates could decrease sertraline plasma concentrations, potentially causing decreased effectiveness of this SSRI.
Sildenafil: (Minor) Sildenafil is metabolized principally by the hepatic CYP3A4 and CYP2C9 isoenzymes. It can be expected that concomitant administration of CYP3A4 enzyme-inducers will decrease plasma levels of sildenafil, however, no interaction studies have been performed. CYP3A4 inducers include barbiturates.
Simvastatin: (Moderate) Barbiturates are significant hepatic CYP3A4 inducers. Monitor for potential reduced cholesterol-lowering efficacy when barbiturates are co-administered with simvastatin, which is metabolized by CYP3A4.
Simvastatin; Sitagliptin: (Moderate) Barbiturates are significant hepatic CYP3A4 inducers. Monitor for potential reduced cholesterol-lowering efficacy when barbiturates are co-administered with simvastatin, which is metabolized by CYP3A4.
Siponimod: (Moderate) Concomitant use of siponimod and butalbital is not recommended for patients with CYP2C9*1/*3 and *2/*3 genotypes due to a significant decrease in siponimod exposure. Use of siponimod with butalbital is not recommended in any patient if they are also receiving a strong CYP3A4 inducer. Siponimod is a CYP2C9 and CYP3A4 substrate; butalbital is a moderate CYP2C9 and CYP3A4 inducer. Across CYP2C9 genotypes, coadministration of a moderate CYP3A4 inducer reduced siponimod exposure by up to 52%, according to in silico evaluation. Coadministration with a moderate CYP2C9/strong CYP3A4 dual inducer decreased siponimod exposure by 57% in CY2C9*1/*1 subjects.
Sirolimus: (Major) Concomitant use of sirolimus and barbiturates should be avoided. Barbiturates such as phenobarbital and primidone may decrease the systemic exposure of sirolimus. Consider alternative agents with less potential for interaction. If concurrent use cannot be avoided, monitor sirolimus plasma concentrations closely and adjust the dose as necessary. Sirolimus is a substrate of CYP3A4; phenobarbital and primidone are potent CYP3A4 inducers. A similar interaction with sirolimus would be expected with all other barbiturates. In addition, the exposure of sirolimus may be altered via P-glycoprotein (P-gp) transport. Sirolimus is P-gp substrate; primidone and phenobarbital may induce P-gp.
Skeletal Muscle Relaxants: (Moderate) Additive CNS depression may occur if barbiturates are used concomitantly with skeletal muscle relaxants. Caution should be exercised during concomitant use of skeletal muscle relaxants and barbiturates; dosage reduction of one or both agents may be necessary.
Sodium Bicarbonate: (Minor) Antacids can delay the oral absorption of acetaminophen, but the interactions are not likely to be clinically significant as the extent of acetaminophen absorption is not appreciably affected.
Sodium Oxybate: (Severe) Sodium oxybate should not be used in combination with CNS depressant anxiolytics, sedatives, and hypnotics or other sedative CNS depressant drugs. Specifically, sodium oxybate use is contraindicated in patients being treated with sedative hypnotic drugs. Sodium oxybate (GHB) has the potential to impair cognitive and motor skills. For example, the concomitant use of barbiturates and benzodiazepines increases sleep duration and may contribute to rapid onset, pronounced CNS depression, respiratory depression, or coma when combined with sodium oxybate. (Moderate) Caffeine should be avoided or used cautiously with sodium oxybate. This combination may be associated with adverse effects such as nervousness, irritability, insomnia, and/or cardiac arrhythmias.
Solifenacin: (Minor) Consuming > 400 mg/day caffeine has been associated with the development of urinary incontinence. Beverages containing caffeine may aggravate bladder symptoms, increase urine output, and counteract the effectiveness of solifenacin to some degree. Patients may wish to limit their intake of caffeinated drugs, dietary supplements, or beverages.
Solriamfetol: (Moderate) Monitor blood pressure and heart rate during coadministration of solriamfetol, a norepinephrine and dopamine reuptake inhibitor, and caffeine. Concurrent use of solriamfetol and other medications that increase blood pressure and/or heart rate may increase the risk of such effects. Coadministration of solriamfetol with other drugs that increase blood pressure or heart rate has not been evaluated.
Spironolactone: (Moderate) Barbiturates, such as butalbital, may potentiate orthostatic hypotension when given concomitantly with spironolactone.
St. John’s Wort, Hypericum perforatum: (Moderate) Inducers of CYP1A2, such as St. John’s wort, Hypericum perforatum, may induce the hepatic oxidative metabolism of caffeine. (Minor) St. John’s wort, Hypericum perforatum induces cytochrome P450 1A2. About 10 to 15% of the acetaminophen dose undergoes oxidative metabolism via cytochrome P450 isoenzymes CYP2E1, 3A4 and 1A2, which produces the hepatotoxic metabolite, N-acetyl-p-benzoquinonimine. Thus, theoretically St. John’s wort might increase the risk of acetaminophen-induced hepatotoxicity by increasing the metabolism of acetaminophen to NAPQI.
Sufentanil: (Major) Concomitant use of sufentanil with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. Because the dose of the sufentanil sublingual tablets cannot be titrated, consider an alternate opiate if barbiturates must be administered. If concurrent use of sufentanil injection is necessary, use the lowest effective doses and minimum treatment durations needed to achieve the desired clinical effect. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concurrent use of sufentanil with barbiturates may decrease sufentanil plasma concentrations, decrease opioid efficacy, and potentially lead to a withdrawal syndrome in those with physical dependence to opioid agonists. Monitor for signs of opioid withdrawal. Discontinuation of barbiturates may increase the risk of increased opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; sufentanil is a CYP3A4 substrate.
Sulfinpyrazone: (Minor) Sulfinpyrazone can induce hepatic oxidative microsomal enzymes and the drug has been shown to increase acetaminophen clearance by roughly 23%. Theoretically, it is thought that the induction of acetaminophen metabolism by sulfinpyrazone may increase the risk of acetaminophen hepatotoxicity due to the formation of increased amounts of toxic acetaminophen metabolites, but there is no confirmatory evidence.
Sunitinib: (Major) Avoid coadministration of butalbital with sunitinib if possible due to decreased exposure to sunitinib which could decrease efficacy. If concomitant use is unavoidable, consider increasing the dose of sunitinib in 12.5 mg increments based on individual safety and tolerability to a maximum of 87.5 mg (GIST and RCC) or 62.5 mg (pNET) daily; monitor carefully for toxicity. The maximum daily dose administered in the pNET study was 50 mg. Sunitinib is a CYP3A4 substrate and butalbital is a moderate CYP3A4 inducer.
Suvorexant: (Moderate) Monitor for decreased efficacy of suvorexant if coadministration with a barbiturate is necessary. Suvorexant is a CYP3A4 substrate and barbiturates are strong CYP3A4 inducers. Coadministration with another strong CYP3A inducer decreased suvorexant exposure by 77% to 88%. Additive CNS effects, such as sedation and psychomotor impairment, are also possible. Dosage adjustments of suvorexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive effects. The use of suvorexant with other drugs to treat insomnia is not recommended. The risk of next-day impairment, including impaired driving, is increased if suvorexant is taken with other CNS depressants. Patients should be cautioned against driving and other activities requiring complete mental alertness. (Minor) Caffeine is a central nervous system (CNS) stimulant. Patients taking medications for sleep, such as suvorexant, eszopiclone, zaleplon, or zolpidem should avoid caffeine-containing medications, dietary supplements, foods, and beverages close to bedtime. Patients should be encouraged to avoid excessive total daily caffeine intake, as part of proper sleep hygiene, since caffeine intake can interfere with proper sleep.
Tacrolimus: (Major) Drugs such as barbiturates, which can induce cytochrome P-450 3A4, may decrease whole blood concentrations of tacrolimus. Monitoring of tacrolimus whole blood concentrations and appropriate dosage adjustments of tacrolimus are recommended.
Tapentadol: (Major) Concomitant use of tapentadol with a barbiturate may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with a barbiturate to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation.
Tasimelteon: (Major) Concurrent use of tasimelteon and strong inducers of CYP3A4, such as barbiturates or primidone, should be avoided. Because tasimelteon is partially metabolized via CYP3A4, a large decrease in exposure is possible with the potential for reduced efficacy. During administration of tasimelteon with another potent inducer of CYP3A4, tasimelteon exposure decreased by about 90%. Barbiturates also induce CYP1A2, a secondary metabolic pathway of tasimelteon. (Minor) Caffeine is a central nervous system (CNS) stimulant. Patients taking melatonin or the melatonin analogs (ramelteon, tasimelteon) for sleep should avoid caffeine-containing medications, dietary supplements, foods, and beverages close to bedtime. Patients should be encouraged to avoid excessive total daily caffeine intake, as part of proper sleep hygiene, since caffeine intake can interfere with proper sleep.
Telaprevir: (Moderate) Close clinical monitoring is advised when administering acetaminophen with telaprevir due to an increased potential for acetaminophen-related adverse events. If acetaminophen dose adjustments are made, re-adjust the dose upon completion of telaprevir treatment. Although this interaction has not been studied, predictions about the interaction can be made based on the metabolic pathway of acetaminophen. Acetaminophen is partially metabolized by the hepatic isoenzyme CYP3A4; telaprevir inhibits this isoenzyme. Coadministration may result in elevated acetaminophen plasma concentrations.
Telotristat Ethyl: (Moderate) Use telotristat ethyl and CYP3A4 substrates, such as acetaminophen, together with caution; the systemic exposure of acetaminophen may be decreased resulting in reduced efficacy. If these drugs are used together, monitor patients for suboptimal efficacy of acetaminophen; consider increasing the dose of acetaminophen if necessary. The systemic exposure of a sensitive CYP3A4 substrate was significantly decreased (by 48%) when it was coadministered with telotristat ethyl. The mechanism of this drug interaction appears to be that telotristat ethyl increases the glucuronidation of the CYP3A4 substrate.
Temazepam: (Moderate) Additive CNS and/or respiratory depression may occur with concurrent use.
Terbinafine: (Moderate) Due to the risk for breakthrough fungal infections, caution is advised when administering terbinafine with barbiturates. Although this interaction has not been studied by the manufacturer, and published literature suggests the potential for interactions to be low, taking these drugs together may decrease the systemic exposure of terbinafine. Predictions about the interaction can be made based on the metabolic pathways of both drugs. Terbinafine is metabolized by at least 7 CYP isoenzymes, with major contributions coming from CYP1A2, CYP2C9, CYP2C19 and CYP3A4; barbiturates induce these enzymes. Monitor patients for breakthrough fungal infections. (Minor) Terbinafine has been shown to inhibit the clearance of caffeine. The clinical significance of this interaction has not been determined.
Terbutaline: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Teriflunomide: (Minor) Monitor for decreased efficacy of caffeine during coadministration of teriflunomide. Teriflunomide may be a weak inducer of CYP1A2. When teriflunomide was given concurrently with caffeine in vivo, a CYP1A2 substrate, the Cmax and AUC of caffeine decreased by 18% and 55%, respectively.
Tetrabenazine: (Moderate) Concurrent use of tetrabenazine and drugs that can cause CNS depression, such as butalbital, can increase both the frequency and the intensity of adverse effects such as drowsiness, sedation, dizziness, and orthostatic hypotension.
Tetracaine: (Moderate) Coadministration of tetracaine with oxidizing agents, such as acetaminophen, may increase the risk of developing methemoglobinemia. Monitor patients closely for signs and symptoms of methemoglobinemia if coadministration is necessary. If methemoglobinemia occurs or is suspected, discontinue tetracaine and any other oxidizing agents. Depending on the severity of symptoms, patients may respond to supportive care; more severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
Thalidomide: (Major) The use of barbiturate anxiolytics, sedatives, or hypnotics with thalidomide may cause an additive sedative effect and should be avoided. Thalidomide frequently causes drowsiness and somnolence. Dose reductions may be required. Patients should be instructed to avoid situations where drowsiness may be a problem and not to take other medications that may cause drowsiness without adequate medical advice. Advise patients as to the possible impairment of mental and/or physical abilities required for the performance of hazardous tasks, such as driving a car or operating other complex or dangerous machinery.
Theophylline, Aminophylline: (Major) Caffeine is a CNS stimulant. The concurrent administration of caffeine to patients taking aminophylline may produce excessive caffeine-like side effects, such as nausea, irritability or nervousness. Adverse effects such as tremors, insomnia, seizures, or cardiac arrhythmias are also possible when excessive dosages of caffeine are taken concurrently. Patients should avoid medications containing caffeine when possible. Patients may also need to limit their intake of caffeine-containing beverages or foods (e.g., coffee, green tea, other teas, colas, or chocolate) to avoid caffeine-like side effects. (Major) Caffeine is a CNS stimulant. The concurrent administration of caffeine to patients taking theophylline may produce excessive caffeine-like side effects, such as nausea, irritability or nervousness. Adverse effects such as tremors, insomnia, seizures, or cardiac arrhythmias are also possible when excessive dosages of caffeine are taken concurrently with theophylline. Patients taking theophylline should avoid medications containing caffeine when possible. Patients may also need to limit their intake of caffeine-containing beverages or foods (e.g., coffee, green tea, other teas, colas, or chocolate) to avoid caffeine-like side effects. In neonates, theophylline is metabolized to caffeine; initiating caffeine after theophylline therapy is halted may result in caffeine toxicity in neonates if serum caffeine levels are not monitored prior to the initiation of caffeine therapy. Concurrent use of theophylline with caffeine in neonates is not recommended due to the potential for additive toxicity. (Moderate) The metabolism of aminophylline can be increased by concurrent use with barbiturates. Patients should be monitored for loss of therapeutic effect if a barbiturate is added is added to aminophylline therapy. Conversely, the hypnotic effects of barbiturates can be reduced by aminophylline. (Moderate) The metabolism of theophylline can be increased by concurrent use with barbiturates. Patients should be monitored for loss of therapeutic effect if a barbiturate is added is added to theophylline therapy. Conversely, the hypnotic effects of barbiturates can be reduced by theophylline.
Thiabendazole: (Moderate) Thiabendazole is a potent inhibitor of CYP1A2 hepatic enzymes. Thiabendazole can interfere with the CYP1A2 metabolism of xanthine derivatives such as caffeine, reducing clearance by up to 50%. Excessive caffeine-related side effects, such as nausea, tremor, or nervousness, may result. Reduction or limitation of the caffeine dosage in medications and limitation of caffeine in beverages and food may be necessary during concomitant treatment.
Thiazide diuretics: (Moderate) Barbiturates may potentiate orthostatic hypotension when used concurrently with thiazide diuretics.
Thiopental: (Minor) Chronic therapy with barbiturates can increase the metabolism and decrease the effectiveness of acetaminophen. During acute overdoses, barbiturates can enhance the formation of toxic acetaminophen metabolites. (Minor) The metabolism of caffeine can be increased by concurrent use with barbiturates. The hypnotic effects of barbiturates can be reduced by caffeine administration.
Thiothixene: (Moderate) Thiothixene can potentiate the CNS-depressant action of the barbiturates. Barbiturates may induce the hepatic metabolism of thiothixene, possibly resulting in decreased neuroleptic effect. Thiothixene does not intensify the anticonvulsant effects of the barbiturates.
Thyroid hormones: (Minor) Hepatic enzyme-inducing drugs, including barbiturates, can increase the catabolism of thyroid hormones. Be alert for a decreased response to thyroid replacement agents with dosage adjustments, discontinuation or addition of barbiturates during thyroid hormone replacement therapy.
Tiotropium; Olodaterol: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Tipranavir: (Major) Barbiturates increase the metabolism of tipranavir, and may lead to decreased efficacy of tipranavir. In addition, tipranavir may inhibit the CYP metabolism of barbiturates, resulting in increased barbiturate concentrations. Appropriate dose adjustments necessary to ensure optimum levels of both anti-retroviral agent and the barbiturate are unknown. Anticonvulsant serum concentrations should be monitored closely if these agents are added; the patient should be observed for changes in the clinical efficacy of the antiretroviral or anticonvulsant regimen
Tizanidine: (Moderate) Concurrent use of tizanidine and CNS depressants like barbiturates can cause additive CNS depression. (Minor) Tizanidine delays the time to attain peak concentrations of acetaminophen by about 16 minutes. The clinical significance of this interaction is unknown.
Tobacco: (Moderate) Inducers of the hepatic CYP450 isoenzyme CYP1A2 may induce the hepatic oxidative metabolism of caffeine. Tobacco smoke contains hydrocarbons that induce hepatic CYP450 microsomal enzymes (e.g., CYP1A1, CYP1A2, CYP2E1). The increased clearance of caffeine by smokers may contribute to the higher consumption of caffeinated beverages reported to occur in this group. Because the effect on hepatic microsomal enzymes is not related to the nicotine component of tobacco, the sudden cessation of tobacco smoking may result in a reduced clearance of caffeine, despite the initiation of a nicotine replacement product. Following several days of abstinence from chronic tobacco smoking, caffeine clearance may decrease by roughly 40%, leading to the possible occurrence of caffeine-related side effects like nausea, nervousness, irritability, tremors, or insomnia, if caffeine use remains the same. (Moderate) Tobacco smoking induces the cytochrome P450 isoenzyme CYP1A2 and may potentially increase the risk for acetaminophen-induced hepatotoxicity during overdose via enhanced generation of acetaminophen’s hepatotoxic metabolite, NAPQI. In one study, current tobacco smoking was found to be very frequent in patients admitted with acetaminophen poisoning. Tobacco smoking appears to be an independent risk factor of severe hepatotoxicity, acute liver failure and death following acetaminophen overdose.
Tolcapone: (Moderate) COMT inhibitors, like entacapone or tolcapone, should be given cautiously with other agents that cause CNS depression due to the possibility of additive sedation. Agents that may cause additive sedation when given concurrently with tolcapone include the barbiturates. The risk for adverse effects may increase, and patients should use caution in driving or other hazardous tasks until the effects of the drugs are known.
Tolterodine: (Minor) Beverages containing caffeine may aggravate bladder symptoms and counteract the effectiveness of tolterodine to some degree. Patients may wish to limit their intake of caffeinated drugs, dietary supplements, or beverages.
Topiramate: (Moderate) Although topiramate is not extensively metabolized (70% renally eliminated), an interaction with barbiturates via hepatic isoenzyme activity is possible. In patients receiving either phenobarbital or primidone in combination with topiramate, there was a < 10% change in phenobarbital or primidone plasma concentrations; the effects on topiramate plasma concentrations were not evaluated. Barbiturates may cause additive sedation or other CNS depressive effects when used concurrently with topiramate. When topiramate is combined with phentermine for the treatment of obesity, a greater risk of CNS depression exists. Concurrent use of topiramate and drugs that cause thrombocytopenia, such as the barbiturates, may also increase the risk of bleeding; monitor patients appropriately.
Tramadol: (Major) Concomitant use of tramadol with barbiturates may cause respiratory depression, hypotension, profound sedation, and death. Limit the use of opioid pain medications with barbiturates to only patients for whom alternative treatment options are inadequate. If concurrent use is necessary, reduce initial dosage and titrate to clinical response; use the lowest effective doses and minimum treatment durations. Educate patients about the risks and symptoms of respiratory depression and sedation. Additionally, concomitant use of tramadol with a barbiturate can decrease tramadol concentrations; this may result in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence. Monitor for reduced efficacy of tramadol and signs of opioid withdrawal. Discontinuation of a barbiturate may increase the risk of seizures, serotonin syndrome, and the risk of opioid-related adverse reactions, such as fatal respiratory depression. Barbiturates induce CYP3A4; tramadol is a CYP3A4 substrate.
Trandolapril; Verapamil: (Major) Barbiturates have been shown to enhance the hepatic clearance of verapamil. The effect on oral verapamil is greater than for IV verapamil, but a significant increase in clearance has been noted for both verapamil dosage forms during concomitant administration of a barbiturate. Patients receiving verapamil should be monitored for loss of therapeutic effect if barbiturates are added. (Minor) Verapamil reduces the clearance of caffeine and increases serum caffeine concentrations, presumably via inhibition of hepatic metabolism. During concomitant therapy with verapamil, it may be prudent to advise patients to limit or minimize the intake of caffeinated products to minimize caffeine-related side effects.
Tranylcypromine: (Major) Additive CNS depression may occur if butalbital is used concomitantly with monoamine oxidase inhibitors. (Major) Excessive use of caffeine in any form should be avoided in patients receiving Monoamine oxidase inhibitors (MAOIs). Limit caffeine intake during MAOI use and for 1 to 2 weeks after discontinuation of any MAOI. the use of non-prescription medicines or dietary supplements containing caffeine should be avoided. Patients should try to avoid or limit the intake of all items containing caffeine such as tea, coffee, chocolate, and cola. Cardiac arrhythmias or severe hypertension may occur because of the potentiation of caffeine’s sympathomimetic effects by MAOIs if caffeine intake is excessive. Ordinarily, selegiline may be an exception, it can only be used safely without dietary restrictions at doses where it presumably selectively inhibits MAO-B (e.g., 10 mg/day). At doses of 20 mg/day, selegiline can interact with foods and beverages. The precise dose at which selegiline becomes a non-selective inhibitor of all MAO is unknown, but may be in the range of 30 to 40 mg per day. Attention to the dose dependent nature of selegiline’s selectivity is critical if it is to be used without elaborate restrictions being placed on diet.
Trazodone: (Major) Monitor for excessive sedation and somnolence during coadministration of trazodone and butalbital. Concurrent use may result in additive CNS depression.
Tretinoin, ATRA: (Moderate) Barbiturates may increase the CYP450 metabolism of tretinoin, ATRA, potentially resulting in decreased plasma concentrations of tretinoin, ATRA. Monitor for decreased clinical effects of tretinoin, ATRA while receiving concomitant therapy.
Triamcinolone: (Moderate) Coadministration may result in decreased exposure to triamcinolone. Butalbital is a CYP3A4 inducer; triamcinolone is a CYP3A4 substrate. Monitor for decreased response to triamcinolone during concurrent use.
Triazolam: (Moderate) Additive CNS and/or respiratory depression may occur. Additionally, barbiturates may increase the metabolism of triazolam. Triazolam is a CYP3A4 substrate. Barbiturates are CYP3A4 inducers.
Tricyclic antidepressants: (Moderate) Tricyclic antidepressants (TCAs), when used concomitantly with anticonvulsants, can increase CNS depression and may also lower the seizure threshold, leading to pharmacodynamic interactions. In addition, pharmacokinetic interactions may occur. Barbiturates may increase TCA metabolism. Monitor patients during concurrent use.
Trimethobenzamide: (Moderate) The concurrent use of trimethobenzamide with barbiturates may potentiate the CNS effects of either trimethobenzamide or the barbiturate.
Trimetrexate: (Moderate) Acetaminophen can inhibit oxidative hepatic enzymes responsible for metabolizing trimetrexate. Concurrent use can decrease the clearance of trimetrexate and thus increase its plasma levels. (Minor) Drugs such as barbiturates can increase the metabolism of trimetrexate by induction of the hepatic cytochrome P-450 system. This can lead to lower plasma concentrations of trimetrexate.
Triprolidine: (Moderate) Additive CNS depression may occur if barbiturates are used concomitantly with triprolidine.
Ulipristal: (Major) Avoid administration of ulipristal with drugs that induce CYP3A4. Ulipristal is a substrate of CYP3A4 and barbiturates (such as phenobarbital or primidone) are CYP3A4 inducers. Concomitant use may decrease the plasma concentration and effectiveness of ulipristal.
Umeclidinium; Vilanterol: (Moderate) Sensitive patients may wish to limit or avoid excessive caffeine intake from foods, beverages, dietary supplements and medications during therapy with beta-agonists. Additive side effects may occur between caffeine and beta-agonists. Caffeine is a CNS-stimulant and beta-agonists are sympathomimetic agents. Sensitive patients might experience tremor, sleep difficulties, or mild increases in heart rate.
Valbenazine: (Major) Co-administration of strong CYP3A4 inducers, such as barbiturates, and valbenazine, a CYP3A4 substrate, is not recommended. Strong CYP3A4 inducers can decrease systemic exposure of valbenazine and its active metabolite compared to the use of valbenazine alone. Reduced exposure of valbenazine and its active metabolite may reduce efficacy.
Valerian, Valeriana officinalis: (Major) Any substances that act on the CNS, including psychoactive drugs and drugs used as anesthetic adjuvants (e.g., barbiturates, benzodiazepines), may theoretically interact with valerian, Valeriana officinalis. The valerian derivative, dihydrovaltrate, binds at barbiturate binding sites; valerenic acid has been shown to inhibit enzyme-induced breakdown of GABA in the brain; the non-volatile monoterpenes (valepotriates) have sedative activity. These interactions are probably pharmacodynamic in nature. There is a possibility of interaction with valerian at normal prescription dosages of anxiolytics, sedatives, and hypnotics (including barbiturates and benzodiazepines). Patients who are taking barbiturates or other sedative/hypnotic drugs should avoid concomitant administration of valerian. Patients taking medications such as tricyclic antidepressants, lithium, MAOIs, skeletal muscle relaxants, SSRIs and serotonin norepinephrine reuptake inhibitors (e.g., duloxetine, venlafaxine) should discuss the use of herbal supplements with their health care professional prior to consuming valerian; combinations should be approached with caution in the absence of clinical data. Patients should not abruptly stop taking their prescribed psychoactive medications.
Valproic Acid, Divalproex Sodium: (Moderate) Valproic acid has been shown to inhibit the hepatic metabolism of phenobarbital. It is likely that other barbiturates, like butalbital, would be affected similarly by valproic acid. Patients should be monitored for an exaggerated barbiturate effect if valproic acid is used concomitantly.
Vardenafil: (Minor) Vardenafil is metabolized by cytochrome P450 3A4. It can be expected that concomitant administration of CYP3A4 enzyme-inducers, such as barbiturates, will decrease plasma levels of vardenafil.
Vemurafenib: (Moderate) Concomitant use of vemurafenib and acetaminophen may result in altered concentrations of acetaminophen. Vemurafenib is an inhibitor of CYP1A2 and CYP2A6, and an inducer of CYP3A4. Acetaminophen is a substrate of CYP1A2, CYP2A6, and CYP3A4. Use caution and monitor patients for toxicity and efficacy.
Verapamil: (Major) Barbiturates have been shown to enhance the hepatic clearance of verapamil. The effect on oral verapamil is greater than for IV verapamil, but a significant increase in clearance has been noted for both verapamil dosage forms during concomitant administration of a barbiturate. Patients receiving verapamil should be monitored for loss of therapeutic effect if barbiturates are added. (Minor) Verapamil reduces the clearance of caffeine and increases serum caffeine concentrations, presumably via inhibition of hepatic metabolism. During concomitant therapy with verapamil, it may be prudent to advise patients to limit or minimize the intake of caffeinated products to minimize caffeine-related side effects.
Vigabatrin: (Moderate) Vigabatrin may cause somnolence and fatigue. Drugs that can cause CNS depression, if used concomitantly with vigabatrin, may increase both the frequency and the intensity of adverse effects such as drowsiness, sedation, and dizziness. Caution should be used when vigabatrin is given with barbiturates.
Vincristine Liposomal: (Major) Vincristine is a substrate for cytochrome P450 (CYP) 3A4. Agents that induce CYP 3A4 may increase the metabolism of vincristine and decrease the efficacy of drug, including barbiturates. Patients receiving these drugs concurrently should be monitored for possible loss of vincristine efficacy.
Vincristine: (Major) Vincristine is a substrate for cytochrome P450 (CYP) 3A4. Agents that induce CYP 3A4 may increase the metabolism of vincristine and decrease the efficacy of drug, including barbiturates. Patients receiving these drugs concurrently should be monitored for possible loss of vincristine efficacy.
Vorapaxar: (Moderate) Use caution during concurrent use of vorapaxar and other barbiturates. Vorapaxar is a CYP3A4 substrate. Barbiturates induce CYP3A. Decreased serum concentrations of vorapaxar and thus decreased efficacy are possible during concurrent use.
Voriconazole: (Severe) Voriconazole is contraindicated for use with long-acting barbiturates, such as butalbital containing products. Barbiturates are CYP3A4 and CYP2C9 inducers and may increase the metabolism and reduce the effective serum concentrations of voriconazole. Barbiturates are also substrates for CYP2C9, and voriconazole may theoretically increase the serum concentrations of the barbiturates.
Vortioxetine: (Major) Patients should be monitored for a decreased response to vortioxetine when barbiturates are co-administered. Vortioxetine is extensively metabolized by CYP isoenzymes, primarily CYP2D6 and by CYP3A4 and other isoenzymes to a lesser extent. The manufacturer recommends that the practitioner consider an increase in dose of vortioxetine when a strong CYP inducer is co-administered for more than 14 days. In such cases, the maximum recommended dose of vortioxetine should not exceed three times the original dose. When the inducer is discontinued, the dose of vortioxetine should be reduced to the original level within 14 days.
Voxelotor: (Major) Avoid coadministration of voxelotor and butalbital as concurrent use may decrease voxelotor exposure and lead to reduced efficacy. If coadministration is unavoidable, increase voxelotor dosage to 2,500 mg PO once daily. Voxelotor is a substrate of CYP3A4; butalbital is a moderate CYP3A4 inducer. Coadministration with another moderate CYP3A4 inducer is predicted to decrease voxelotor exposure by up to 60%.
Warfarin: (Major) A serious drug interaction can occur between barbiturates and warfarin. All barbiturates are hepatic enzyme inducers and the clinical effects of warfarin can be compromised if a barbiturate is added. More importantly, discontinuation of a barbiturate during warfarin therapy has lead to fatal bleeding episodes when the hepatic enzyme-inducing properties of the barbiturate subside. Clinicians should note that warfarin doses will require readjustment if a barbiturate is added or discontinued during warfarin therapy. Dosage adjustments of warfarin may be necessary within 2 weeks of beginning barbiturate treatment, but the effect of the barbiturate on warfarin metabolism may persist for more than a month after discontinuing the barbiturate. (Minor) Although acetaminophen is routinely considered safer than aspirin and agent of choice when a mild analgesic/antipyretic is necessary for a patient receiving therapy with warfarin, acetaminophen has also been shown to augment the hypoprothrombinemic response to warfarin. Concomitant acetaminophen ingestion may result in increases in the INR in a dose-related fashion. Clinical bleeding has been reported. Single doses or short (i.e., several days) courses of treatment with acetaminophen are probably safe in most patients taking warfarin. Clinicians should be alert for an increased INR if acetaminophen is administered in large daily doses for longer than 10 to 14 days.
Yohimbine: (Moderate) Dangerous cardiac arrhythmias or severe hypertension can occur because of the potentiation of caffeine’s sympathomimetic effects by drugs with MAOI activity such as high doses of yohimbine.
Zaleplon: (Major) Coadministration of zaleplon and barbiturates may result in additive CNS depression. Caution should be exercised during concomitant use of anxiolytics, sedatives, and hypnotics and any barbiturate. In addition, zaleplon is partially metabolized by CYP3A4, and concurrent use of strong CYP3A4 inducers, such as barbiturates, may increase the clearance of zaleplon. Dosage adjustments should be made on an individual basis according to efficacy and tolerability. (Minor) Caffeine is a central nervous system (CNS) stimulant. Patients taking medications for sleep, such as zaleplon should avoid caffeine-containing medications, dietary supplements, foods, and beverages close to bedtime. Patients should be encouraged to avoid excessive total daily caffeine intake, as part of proper sleep hygiene, since caffeine intake can interfere with proper sleep.
Zanubrutinib: (Major) Avoid the concomitant use of zanubrutinib and butalbarbital. Coadministration may result in decreased zanubrutinib exposure and reduced efficacy. Zanubrutinib is a CYP3A4 substrate; butalbarbital is a moderate CYP3A4 inducer. The AUC of zanubrutinib is predicted to decrease by 60% when coadministered with another moderate CYP3A4 inducer.
Ziconotide: (Moderate) CNS depressant medications, such as barbiturates, may increase drowsiness, dizziness, and confusion that are associated with ziconotide. Dosage adjustments may be necessary if ziconotide is used with a barbiturate.
Zidovudine, ZDV: (Minor) Both acetaminophen and zidovudine, ZDV undergo glucuronidation. Competition for the metabolic pathway is thought to have caused a case of acetaminophen-related hepatotoxicity. This interaction may be more clinically significant in patients with depleted glutathione stores, such as patients with acquired immunodeficiency syndrome, poor nutrition, or alcoholism.
Zileuton: (Moderate) Inhibitors of CYP1A2, such as zileuton, may inhibit the hepatic oxidative metabolism of caffeine. No specific management is recommended except in patients who complain of caffeine-related side effects like nausea, tremor, or palpitations. In such patients, the dosage of caffeine-containing medications or the ingestion of caffeine-containing products may need to be reduced.
Ziprasidone: (Major) Ziprasidone is partially metabolized via the hepatic CYP3A4 isoenzyme. A decrease in ziprasidone plasma levels could potentially occur if the drug is used concurrently with inducers of CYP3A4 including barbiturates. Additive CNS depressant effects are also possible when ziprasidone is used concurrently with barbiturates.
Zolmitriptan: (Minor) Zolmitriptan can delay the Tmax of acetaminophen by one hour. A single 1 g dose of acetaminophen does not alter the pharmacokinetics of zolmitriptan and its active metabolite. The interaction between zolmitriptan and acetaminophen is not likely to be clinically significant.
Zolpidem: (Major) Concurrent use of zolpidem with barbiturates should be avoided if possible due to additive CNS depression. Sleep-related behaviors, such as sleep-driving, are more likely to occur during concurrent use of zolpidem and other CNS depressants than zolpidem alone. Concurrent use of zolpidem with other sedative-hypnotics at bedtime or in the middle of the night is not recommended. Dosage reduction may be required for co-use in some patients. For example, a dosage reduction of the Intermezzo brand of sublingual zolpidem tablets to 1.75 mg/night is recommended when used with another CNS depressant. Barbiturates are CYP3A4 enzyme inducers and may cause decreased plasma concentrations of zolpidem; in some patients efficacy may be reduced. CYP3A4 is the primary isoenzyme responsible for zolpidem metabolism, and there is evidence of significant decreases in systemic exposure and pharmacodynamic effects of zolpidem during coadministration of a potent CYP3A4 inducer. (Minor) Caffeine is a central nervous system (CNS) stimulant. Patients taking medications for sleep, such as zolpidem should avoid caffeine-containing medications, dietary supplements, foods, and beverages within the hours close to bedtime. Patients should be encouraged to avoid excessive total daily caffeine intake, as part of proper sleep hygiene, since caffeine intake can interfere with proper sleep. However, in healthy subjects (without insomnia) in a pharmacokinetic study, coadministration of caffeine at a dosage of 150 to 300 mg with zolpidem did not counteract the sedative effects of a single 10 mg dose of zolpidem.
Zonisamide: (Moderate) Zonisamide is metabolized by hepatic cytochrome P450 enzyme 3A4. Barbiturates are inducers of CYP3A4 and can reduce the systemic exposure to zonisamide by increasing the metabolism of the drug.
PREGNANCY AND LACTATION
Acetaminophen; butalbital; caffeine components may all be excreted to some extent into breast milk. According to the manufacturer, because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug. Caffeine can accumulate in the neonate. Chronic barbiturate use while breast-feeding may cause dependence in the neonate. The chronic use of acetaminophen; butalbital; caffeine during breast-feeding is not recommended. Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breast-feeding infant experiences an adverse effect related to a maternally ingested drug, healthcare providers are encouraged to report the adverse effect to the FDA.
MECHANISM OF ACTION
Acetaminophen is an analgesic; butalbital is added in combination with acetaminophen due to its CNS depressive (sedative) properties; caffeine is a methylxanthine CNS psychostimulant. The role each component plays in the relief of tension headache symptoms is incompletely understood.
Acetaminophen: Acetaminophen acts primarily in the CNS and increases the pain threshold by inhibiting cyclooxygenase, an enzyme involved in prostaglandin (PG) synthesis. Acetaminophen inhibits both isoforms of central cyclooxygenase, COX-1 and COX-2. Acetaminophen does not inhibit PG synthesis in peripheral tissues, which is the reason for its lack of peripheral anti-inflammatory effects.
Butalbital: Barbiturates inhibit ascending conduction in the reticular formation, which interferes with conduction of impulses to the cortex causing sensory cortex depression, decreased motor activity, drowsiness, sedation and changes in cerebral function. Barbiturates bind to gamma-aminobutyric acid (GABA) A and alpha-amino-3-hydroxy-5-methyl-isoxazole-4-propionic acid (AMPA) receptors. GABA A receptor binding by barbiturates causes inhibition of the postsynaptic neuron, as the physiologic substrate for the receptor is GABA, which is an inhibitory amino acid. Barbiturates enhance GABA binding to GABA A receptors, which prolongs the duration of GABA-induced chloride channel opening and promotes binding of a benzodiazepine to the GABA A receptor. Benzodiazepines increase the frequency of GABA-induced chloride channel opening. Thus, additive CNS depressant effects occur with concomitant barbiturate and benzodiazepine usage. Binding of a barbiturate to the AMPA receptor prevents the binding of the physiologic substrate, AMPA, an excitatory amino acid. The activation of GABA A receptors and the inhibition of AMPA receptors causes a nonselective depressant effect throughout the CNS that can range from mild sedation to general anesthesia. Butalbital does not have a direct analgesic action; pain perception is relatively unimpaired until the moment of unconsciousness. Thus, butalbital has a low therapeutic index.
Caffeine: Caffeine causes cerebral vasoconstriction, which decreases blood flow and oxygen tension. In combination with acetaminophen, caffeine may provide a quicker onset of action and enhance pain relief allowing for lower doses of analgesics. In some patients, caffeine relieves headaches by treating the effects of caffeine withdrawal.
PHARMACOKINETICS
Acetaminophen-butalbital-caffeine is administered orally.
Acetaminophen: Acetaminophen is metabolized in the liver via glucuronidation and sulfate conjugation and is excreted in the urine as glutathione and sulfate conjugates. However about 10—15% of the acetaminophen dose undergoes oxidative metabolism via cytochrome P450 isoenzymes (CYP) 2E1 and 1A2 and then glucuronidation to cysteine and mercapturic acid conjugates. In cases of glucuronide depletion, such as acetaminophen overdose, a hepatotoxic metabolite is formed. The half-life of acetaminophen in patients with normal hepatic function is 2—4 hours.
Butalbital: Butalbital is metabolized by the hepatic microsomal system and has a half-life of 35 hours. Butalbital induces hepatic enzymes but to a lesser degree than phenobarbital. Butalbital is renally eliminated as metabolites and unchanged drug (3—4%).
Caffeine: Caffeine undergoes hepatic metabolism to paraxanthine, theobromine, and theophylline. Elimination of caffeine is renal as inactive metabolites. The elimination half-life of caffeine in adults is 3—7 hours.
All three components are well absorbed from the GI tract. During migraines gastric stasis may occur which could alter the pharmacokinetic parameters of these agents. Time to onset of analgesia is about 1—2 hours
