Make sure you tell your doctor about your complete medical history when he/she is prescribing this drug to you. This drug might not be suitable for you if you are suffering from kidney, liver or heart diseases. You should also inform your doctor if you have an allergic reaction to gabapentin. Avoid having alcohol while you are on this medicine. Antacids can interfere with the absorption of Neurontin; therefore, it is advisable not to have Antacids at least 2 hours before having this medicine. In case you are pregnant or are planning to become pregnant, do not forget to inform the same to your doctor. Doctors do not generally prescribe this drug to pregnant ladies unless there is an immediate and genuine need for it.
This medicine is not meant for children below the age of 12 years. Many people experience side effects like blurred vision and drowsiness after taking this drug. Therefore, it is advisable not to drive after taking the medicine. Allow your body to get adapted to this new drug. Visit the doctor frequently as he/she will want to carry out regular tests to see how your body is adapting to this drug.
Drug Reaction With Eosinophilia And Systemic Symptoms (DRESS)/Multiorgan Hypersensitivity
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), also known as multiorgan hypersensitivity, has occurred with NEURONTIN. Some of these reactions have been fatal or life-threatening. DRESS typically, although not exclusively, presents with fever, rash, and/or lymphadenopathy, in association with other organ system involvement, such as hepatitis,nephritis, hematological abnormalities, myocarditis, or myositis sometimes resembling an acute viral infection. Eosinophilia is often present. This disorder is variable in its expression, and other organ systems not noted here may be involved.
It is important to note that early manifestations of hypersensitivity, such as fever or lymphadenopathy, may be present even though rash is not evident. If such signs or symptoms are present, the patient should be evaluated immediately. NEURONTIN should be discontinued if an alternative etiologyfor the signs or symptoms cannot be established.
Anaphylaxis And Angioedema
NEURONTIN can cause anaphylaxis and angioedema after the first dose or at any time during treatment. Signs and symptoms in reported cases have included difficulty breathing, swelling of the lips, throat, and tongue, andhypotension requiring emergency treatment. Patients should be instructed to discontinue NEURONTIN and seek immediate medical care should they experience signs or symptoms of anaphylaxis or angioedema.
Effects On Driving and Operating Heavy Machinery
Patients taking NEURONTIN should not drive until they have gained sufficient experience to assess whether NEURONTIN impairs their ability to drive. Driving performance studies conducted with a prodrug of gabapentin (gabapentin enacarbil tablet, extended release) indicate that gabapentin may cause significant driving impairment. Prescribers and patients should be aware that patients’ ability to assess their own driving competence, as well as their ability to assess the degree of somnolence caused by NEURONTIN, can be imperfect. The duration of driving impairment after starting therapy with NEURONTIN is unknown. Whether the impairment is related to somnolence or other effects of NEURONTIN is unknown.
Moreover, because NEURONTIN causes somnolence and dizziness , patients should be advised not to operate complex machinery until they have gained sufficient experience on NEURONTIN to assess whether NEURONTIN impairs their ability to perform such tasks.
Somnolence/Sedation And Dizziness
During the controlled epilepsy trials in patients older than 12 years of age receiving doses of NEURONTIN up to 1800 mg daily, somnolence, dizziness, and ataxia were reported at a greater rate in patients receiving NEURONTIN compared to placebo: i.e., 19% in drug versus 9% in placebo for somnolence, 17% in drug versus 7% in placebo for dizziness, and 13% in drug versus 6% in placebo for ataxia. In these trials somnolence, ataxia and fatigue were common adverse reactions leading to discontinuation of NEURONTIN in patients older than 12 years of age, with 1.2%, 0.8% and 0.6% discontinuing for these events, respectively.
During the controlled trials in patients with post-herpetic neuralgia, somnolence and dizziness were reported at a greater rate compared to placebo in patients receiving NEURONTIN, in dosages up to 3600 mg per day: i.e., 21% in NEURONTIN-treated patients versus 5% in placebo-treated patients for somnolence and 28% in NEURONTIN-treated patients versus 8% in placebo-treated patients for dizziness. Dizziness and somnolence were among the most common adverse reactions leading to discontinuation of NEURONTIN.
Patients should be carefully observed for signs of central nervous system(CNS) depression, such as somnolence and sedation, when NEURONTIN is used with other drugs with sedative properties because of potential synergy. In addition, patients who require concomitant treatment with morphine may experience increases in gabapentin concentrations and may require dose adjustment.
Withdrawal Precipitated Seizure, Status Epilepticus
Antiepileptic drugs should not be abruptly discontinued because of the possibility of increasing seizure frequency.
In the placebo-controlled epilepsy studies in patients > 12 years of age, the incidence of status epilepticus in patients receiving NEURONTIN was 0.6% (3 of 543) vs. 0.5% in patients receiving placebo (2 of 378). Among the 2074 patients > 12 years of age treated with NEURONTIN across all epilepsy studies (controlled and uncontrolled), 31 (1.5%) had status epilepticus. Of these, 14 patients had no prior history of status epilepticus either before treatment or while on other medications. Because adequate historical data are not available, it is impossible to say whether or not treatment with NEURONTIN is associated with a higher or lower rate of status epilepticus than would be expected to occur in a similar population not treated with NEURONTIN.
Suicidal Behavior And Ideation
Antiepileptic drugs (AEDs), including NEURONTIN, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5-100 years) in the clinical trials analyzed. Table 2 shows absolute and relative risk by indication for all evaluated AEDs.
TABLE 2 : Risk by Indication for Antiepileptic Drugs in the Pooled Analysis
| INDICATION | PLACEBO PATIENTS WITH EVENTS PER 1000 PATIENTS | DRUG PATIENTS WITH EVENTS PER 1000 PATIENTS | RELATIVE RISK: INCIDENCE OF EVENTS IN DRUG PATIENTS/INCIDENCE IN PLACEBO PATIENTS | RISK DIFFERENCE: ADDITIONAL DRUG PATIENTS WITH EVENTS PER 1000 PATIENTS |
| Epilepsy | 1.0 | 3.4 | 3.5 | 2.4 |
| Psychiatric | 5.7 | 8.5 | 1.5 | 2.9 |
| Other | 1.0 | 1.8 | 1.9 | 0.9 |
| Total | 2.4 | 4.3 | 1.8 | 1.9 |
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing NEURONTIN or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Neuropsychiatric Adverse Reactions (Pediatric Patients 3-12 Years of Age)
Gabapentin use in pediatric patients with epilepsy 3-12 years of age is associated with the occurrence of central nervous system related adverse reactions. The most significant of these can be classified into the following categories: 1) emotional lability (primarily behavioral problems), 2) hostility, including aggressive behaviors, 3) thought disorder, including concentration problems and change in school performance, and 4) hyperkinesia (primarily restlessness and hyperactivity). Among the gabapentin-treated patients, most of the reactions were mild to moderate in intensity.
In controlled clinical epilepsy trials in pediatric patients 3–12 years of age, the incidence of these adverse reactions was: emotional lability 6% (gabapentin-treated patients) vs. 1.3% (placebotreated patients); hostility 5.2% vs. 1.3%; hyperkinesia 4.7% vs. 2.9%; and thought disorder 1.7% vs. 0%. One of these reactions, a report of hostility, was considered serious. Discontinuation of gabapentin treatment occurred in 1.3% of patients reporting emotional lability and hyperkinesia and 0.9% of gabapentin-treated patients reporting hostility and thought disorder. One placebo-treated patient (0.4%) withdrew due to emotional lability.
Tumorigenic Potential
In an oral carcinogenicity study, gabapentin increased the incidence of pancreatic acinar cell tumors in rats . The clinical significance of this finding is unknown. Clinical experience during gabapentin’s premarketing development provides no direct means to assess its potential for inducing tumors in humans.
In clinical studies in adjunctive therapy in epilepsy comprising 2085 patient-years of exposure in patients > 12 years of age, new tumors were reported in 10 patients (2 breast, 3 brain, 2 lung, 1 adrenal, 1 non-Hodgkin’s lymphoma, 1 endometrial carcinoma in situ), and preexisting tumors worsened in 11 patients (9 brain, 1 breast, 1 prostate) during or up to 2 years following discontinuation of NEURONTIN. Without knowledge of the background incidence and recurrence in a similar population not treated with NEURONTIN, it is impossible to know whether the incidence seen in this cohort is or is not affected by treatment.
Sudden And Unexplained Death In Patients With Epilepsy
During the course of premarketing development of NEURONTIN, 8 sudden and unexplained deaths were recorded among a cohort of 2203 epilepsy patients treated (2103 patient-years of exposure) with NEURONTIN.
Some of these could represent seizure-related deaths in which the seizure was not observed, e.g., at night. This represents an incidence of 0.0038 deaths per patient-year. Although this rate exceeds that expected in a healthy population matched for age and sex, it is within the range of estimates for the incidence of sudden unexplained deaths in patients with epilepsy not receiving NEURONTIN (ranging from 0.0005 for the general population of epileptics to 0.003 for a clinical trial population similar to that in the NEURONTIN program, to 0.005 for patients with refractory epilepsy). Consequently, whether these figures are reassuring or raise further concern depends on comparability of the populations reported upon to the NEURONTIN cohort and the accuracy of the estimates provided.
Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Administration Information
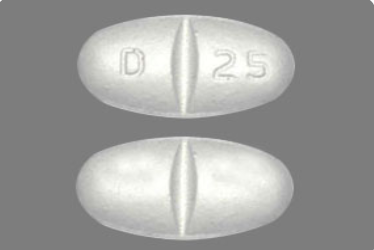
Inform patients that NEURONTIN is taken orally with or without food. Inform patients that, should they divide the scored 600 mg or 800 mg tablet in order to administer a half-tablet, they should take the unused half-tablet as the next dose. Advise patients to discard half-tablets not used within 28 days of dividing the scored tablet.
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multiorgan Hypersensitivity
Prior to initiation of treatment with NEURONTIN, instruct patients that a rash or other signs or symptoms of hypersensitivity (such as fever or lymphadenopathy) may herald a serious medical event and that the patient should report any such occurrence to a physician immediately .
Anaphylaxis and Angioedema
Advise patients to discontinue NEURONTIN and seek medical care if they develop signs or symptoms of anaphylaxis or angioedema .
Dizziness and Somnolence and Effects on Driving and Operating Heavy Machinery
Advise patients that NEURONTIN may cause dizziness, somnolence, and other symptoms and signs of CNS depression. Other drugs with sedative properties may increase these symptoms. Accordingly, although patients’ ability to determine their level of impairment can be unreliable, advise them neither to drive a car nor to operate other complex machinery until they have gained sufficient experience on NEURONTIN to gauge whether or not it affects their mental and/or motor performance adversely. Inform patients that it is not known how long this effect lasts.
Suicidal Thinking and Behavior
Counsel the patient, their caregivers, and families that AEDs, including NEURONTIN, may increase the risk of suicidal thoughts and behavior. Advise patients of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Instruct patients to report behaviors of concern immediately to healthcare providers .
Use in Pregnancy
Instruct patients to notify their physician if they become pregnant or intend to become pregnant during therapy, and to notify their physician if they arebreast feeding or intend to breast feed during therapy
Encourage patients to enroll in the NAAED Pregnancy Registry if they become pregnant. This registry is collecting information about the safety of antiepileptic drugs during pregnancy. To enroll, patients can call the toll free number 1-888-233-2334
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment Of Fertility
 Gabapentin was administered orally to mice and rats in 2-year carcinogenicity studies. No evidence of drug-related carcinogenicity was observed in mice treated at doses up to 2000 mg/kg/day. At 2000 mg/kg, the plasma gabapentin exposure (AUC) in mice is approximately 2 times that in humans at the MRHD of 3600 mg/day. In rats, increases in the incidence of pancreatic acinar cell adenoma and carcinoma were found in male rats receiving the highest dose (2000 mg/kg), but not at doses of 250 or 1000 mg/kg/day. At 1000 mg/kg, the plasma gabapentin exposure (AUC) in rats is approximately 5 times that in humans at the MRHD.
Gabapentin was administered orally to mice and rats in 2-year carcinogenicity studies. No evidence of drug-related carcinogenicity was observed in mice treated at doses up to 2000 mg/kg/day. At 2000 mg/kg, the plasma gabapentin exposure (AUC) in mice is approximately 2 times that in humans at the MRHD of 3600 mg/day. In rats, increases in the incidence of pancreatic acinar cell adenoma and carcinoma were found in male rats receiving the highest dose (2000 mg/kg), but not at doses of 250 or 1000 mg/kg/day. At 1000 mg/kg, the plasma gabapentin exposure (AUC) in rats is approximately 5 times that in humans at the MRHD.
Studies designed to investigate the mechanism of gabapentin-induced pancreatic carcinogenesis in rats indicate that gabapentin stimulates DNA synthesis in rat pancreatic acinar cells in vitro and, thus, may be acting as a tumor promoter by enhancing mitogenic activity. It is not known whether gabapentin has the ability to increase cell proliferation in other cell types or in other species, including humans.
Gabapentin did not demonstrate mutagenic or genotoxic potential in three in vitro and four in vivo assays. It was negative in the Ames test and the in vitroHGPRT forward mutation assay in Chinese hamster lung cells; it did not produce significant increases in chromosomal aberrations in the in vitroChinese hamster lung cell assay; it was negative in the in vivo chromosomal aberration assay and in the in vivo micronucleus test in Chinese hamster bone marrow; it was negative in the in vivo mouse micronucleus assay; and it did not induce unscheduled DNA synthesis in hepatocytes from rats given gabapentin.
No adverse effects on fertility or reproduction were observed in rats at doses up to 2000 mg/kg. At 2000 mg/kg, the plasma gabapentin exposure (AUC) in rats is approximately 8 times that in humans at the MRHD.
Use In Specific Populations
Pregnancy
Pregnancy Category C
There are no adequate and well-controlled studies in pregnant women. In nonclinical studies in mice, rats, and rabbits, gabapentin was developmentally toxic when administered to pregnant animals at doses similar to or lower than those used clinically. NEURONTIN should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
When pregnant mice received oral doses of gabapentin (500, 1000, or 3000 mg/kg/day) during the period of organogenesis, embryo-fetal toxicity (increased incidences of skeletal variations) was observed at the two highest doses. The no-effect dose for embryo-fetal developmental toxicity in mice was 500 mg/kg/day or approximately ½ of the maximum recommended human dose (MRHD) of 3600 mg/kg on a body surface area (mg/m²) basis.
In studies in which rats received oral doses of gabapentin (500 to 2000 mg/kg/day), during pregnancy, adverse effect on offspring development (increased incidences of hydroureter and/or hydronephrosis) were observed at all doses. The lowest effect dose for developmental toxicity in rats is approximately equal to the MRHD on a mg/m² basis.
When pregnant rabbits were treated with gabapentin during the period of organogenesis, an increase in embryo-fetal mortality was observed at all doses tested (60, 300, or 1500 mg/kg). The lowest effect dose for embryo-fetal developmental toxicity in rabbits is less than the MRHD on a mg/m² basis.
In a published study, gabapentin (400 mg/kg/day) was administered byintraperitoneal injection to neonatal mice during the first postnatal week, a period of synaptogenesis in rodents (corresponding to the last trimester of pregnancy in humans). Gabapentin caused a marked decrease in neuronal synapse formation in brains of intact mice and abnormal neuronal synapse formation in a mouse model of synaptic repair. Gabapentin has been shownin vitro to interfere with activity of the α2δ subunit of voltage-activated calcium channels, a receptor involved in neuronal synaptogenesis. The clinical significance of these findings is unknown.
To provide information regarding the effects of in utero exposure to NEURONTIN, physicians are advised to recommend that pregnant patients taking NEURONTIN enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry. This can be done by calling the toll free number 1-888-233-2334, and must be done by patients themselves. Information on the registry can also be found at the website http://www.aedpregnancyregistry.org/.
Nursing Mothers
Gabapentin is secreted into human milk following oral administration. A nursed infant could be exposed to a maximum dose of approximately 1 mg/kg/day of gabapentin. Because the effect on the nursing infant is unknown, NEURONTIN should be used in women who are nursing only if the benefits clearly outweigh the risks.
Pediatric Use
Safety and effectiveness of NEURONTIN in the management of postherpetic neuralgia in pediatric patients have not been established.
Effectiveness as adjunctive therapy in the treatment of partial seizures in pediatric patients below the age of 3 years has not been established
Geriatric Use
The total number of patients treated with NEURONTIN in controlled clinical trials in patients with postherpetic neuralgia was 336, of which 102 (30%) were 65 to 74 years of age, and 168 (50%) were 75 years of age and older. There was a larger treatment effect in patients 75 years of age and older compared with younger patients who received the same dosage. Since gabapentin is almost exclusively eliminated by renal excretion, the larger treatment effect observed in patients ≥ 75 years may be a consequence of increased gabapentin exposure for a given dose that results from an age-related decrease in renal function. However, other factors cannot be excluded. The types and incidence of adverse reactions were similar across age groups except for peripheral edema and ataxia, which tended to increase in incidence with age.
Clinical studies of NEURONTIN in epilepsy did not include sufficient numbers of subjects aged 65 and over to determine whether they responded differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and dose should be adjusted based on creatinine clearance values in these patients
Fioricet Precautions
It is very important that your doctor check your progress at regular visits, especially in the first few months if you have epilepsy. This will allow your doctor to see if the medicine is working properly and to decide if you should continue to take it.
Check with your doctor right away if you have a fever, rash, swollen, painful, or tender lymph glands in the neck, armpit, or groin, unusual bleeding or bruising, or yellow eyes or skin. These may be symptoms of a serious and life-threatening allergic reaction called drug reaction with eosinophilia and systemic symptoms (DRESS) or multiorgan hypersensitivity.
This medicine may cause serious allergic reactions, including anaphylaxis and angioedema, which can be life-threatening and require immediate medical attention. Call your doctor right away if you have a rash, itching, trouble breathing, trouble swallowing, or any swelling of your hands, face, or mouth while you are using this medicine.
Gabapentin may cause vision changes, clumsiness, unsteadiness, dizziness, drowsiness, sleepiness, or trouble with thinking. Make sure you know how you react to this medicine before you drive, use machines, or do anything else that could be dangerous if you are not alert, well-coordinated, or able to think or see well. If these side effects are especially bothersome, check with your doctor.
This medicine may cause some people to be agitated, irritable, or display other abnormal behaviors, such as feeling sad or hopeless, getting upset easily, or feeling nervous, restless, or hostile. It may also cause some people to have suicidal thoughts and tendencies or to become more depressed. If you, your child, or your caregiver notice any of these side effects, tell your doctor right away.
This medicine will add to the effects of alcohol and other CNS depressants (medicines that make you drowsy or less alert). Some examples of CNS depressants are antihistamines or medicine for hay fever, allergies, or colds, sedatives, tranquilizers, or sleeping medicines, prescription pain medicine or narcotics, other medicines for seizures (eg, barbiturates), muscle relaxants, or anesthetics, including some dental anesthetics. Check with your medical doctor or dentist before taking any of the above while you or your child are using gabapentin.
This medicine may cause respiratory depression, a serious breathing problem that can be life-threatening, when used together with narcotic pain medicines. Check with your doctor right away if you have pale or blue lips, fingernails, or skin, difficult or trouble breathing, or irregular, fast or slow, or shallow breathing.
Do not stop using gabapentin without checking with your doctor. Stopping the medicine suddenly may cause seizures. Your doctor may want you or your child to gradually reduce the amount you are taking before stopping it completely.
Make sure any doctor or dentist who treats you knows that you are using this medicine. This medicine may affect the results of certain medical tests.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Drug Interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Acepromazine
- Alfentanil
- Alprazolam
- Amobarbital
- Anileridine
- Aripiprazole
- Asenapine
- Baclofen
- Benperidol
- Benzhydrocodone
- Bromazepam
- Buprenorphine
- Buspirone
- Butabarbital
- Butorphanol
- Calcifediol
- Calcium Oxybate
- Cannabidiol
- Cannabis
- Carbinoxamine
- Carisoprodol
- Carphenazine
- Chloral Hydrate
- Chlordiazepoxide
- Chlorpromazine
- Chlorzoxazone
- Clobazam
- Clonazepam
- Clorazepate
- Clozapine
- Codeine
- Cyclobenzaprine
- Daridorexant
- Dexmedetomidine
- Diacetylmorphine
- Diazepam
- Dichloralphenazone
- Difenoxin
- Dihydrocodeine
- Diphenhydramine
- Diphenoxylate
- Doxylamine
- Droperidol
- Enflurane
- Esketamine
- Estazolam
- Eszopiclone
- Ethchlorvynol
- Ethopropazine
- Ethylmorphine
- Fentanyl
- Flibanserin
- Flunitrazepam
- Fluphenazine
- Flurazepam
- Fluspirilene
- Fospropofol
- Gabapentin Enacarbil
- Halazepam
- Haloperidol
- Halothane
- Hexobarbital
- Hydrocodone
- Hydromorphone
- Hydroxyzine
- Isoflurane
- Ketamine
- Ketazolam
- Ketobemidone
- Lacosamide
- Levocetirizine
- Levorphanol
- Lorazepam
- Loxapine
- Magnesium Oxybate
- Meclizine
- Melperone
- Meperidine
- Mephobarbital
- Meprobamate
- Meptazinol
- Mesoridazine
- Metaxalone
- Methadone
- Methdilazine
- Methocarbamol
- Methohexital
- Methotrimeprazine
- Methylene Blue
- Midazolam
- Molindone
- Moricizine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Nicomorphine
- Nitrazepam
- Nitrous Oxide
- Olanzapine
- Oliceridine
- Opium
- Opium Alkaloids
- Orlistat
- Orphenadrine
- Oxazepam
- Oxycodone
- Oxymorphone
- Papaveretum
- Paregoric
- Pentazocine
- Pentobarbital
- Perampanel
- Perazine
- Periciazine
- Perphenazine
- Phenobarbital
- Pimozide
- Piperacetazine
- Pipotiazine
- Piritramide
- Potassium Oxybate
- Prazepam
- Pregabalin
- Primidone
- Prochlorperazine
- Promazine
- Promethazine
- Propofol
- Quazepam
- Quetiapine
- Ramelteon
- Remifentanil
- Remimazolam
- Remoxipride
- Ropeginterferon Alfa-2b-njft
- Secobarbital
- Sertindole
- Sodium Oxybate
- Sufentanil
- Sulpiride
- Suvorexant
- Tapentadol
- Temazepam
- Thiethylperazine
- Thiopental
- Thiopropazate
- Thioridazine
- Tilidine
- Tizanidine
- Tolonium Chloride
- Topiramate
- Tramadol
- Triazolam
- Trifluoperazine
- Trifluperidol
- Triflupromazine
- Trimeprazine
- Zaleplon
- Zolpidem
- Zopiclone
- Zotepine
- Zuranolone
Using this medicine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Aluminum Carbonate, Basic
- Aluminum Hydroxide
- Aluminum Phosphate
- Dihydroxyaluminum Aminoacetate
- Dihydroxyaluminum Sodium Carbonate
- Ginkgo
- Magaldrate
- Magnesium Carbonate
- Magnesium Hydroxide
- Magnesium Oxide
- Magnesium Trisilicate
