When you have diabetes, high blood sugar levels can damage nerves and blood vessels.
The nerves and blood vessels supplying the feet are long and delicate. Because of that, the feet — and especially the toes — often get affected first.
Damage to the nerves and blood vessels in the feet causes two separate but related problems: peripheral neuropathy and peripheral artery disease. Together, they can lead to foot pain and complications.
Treating foot pain caused by diabetes focuses on addressing the underlying nerve damage, alleviating symptoms, and preventing further complications.
peripheral neuropathy and peripheral artery disease
1. Peripheral neuropathy
This is the name for damage to any nerves outside the brain and spinal cord. When it happens in the feet and legs, peripheral neuropathy causes pain, numbness, and other problems related to balance and foot stability.
2. Peripheral artery disease
This is when damage to blood vessel walls causes blood vessels to become stiff and narrow. This can lower blood flow to the feet, which, in turn, leads to:
-
Breakdown of the skin, making it more prone to damage and infection
-
Slower healing of injuries
-
Greater risk of infection, ulcers, and gangrene
How to Treat Your Foot Pain Caused by Diabets
Here’s a comprehensive guide:
1. Optimize Blood Sugar Control
- Why It Helps: Keeping blood sugar levels within target ranges slows the progression of nerve damage and may reduce pain over time.
- How to Achieve It:
- Monitor blood sugar levels regularly.
- Follow your doctor’s recommended treatment plan, which may include insulin or oral medications like metformin.
- Maintain an A1C level below 7%, or as advised by your healthcare provider.
2. Medications for Pain Management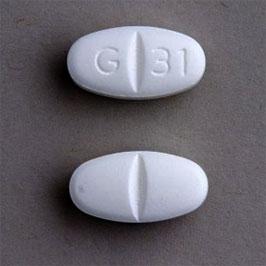
Oral Medications
- Gabapentin or Pregabalin: Effective for neuropathic pain by reducing nerve signal overactivity.
- Duloxetine (Cymbalta): An antidepressant that also works for nerve pain.
- Amitriptyline or Nortriptyline: Tricyclic antidepressants sometimes used for pain relief.
- Pain Relievers: Over-the-counter options like acetaminophen or ibuprofen may help with mild discomfort, though they are less effective for neuropathic pain.
Topical Treatments
- Capsaicin Cream: Derived from chili peppers, it can reduce localized nerve pain.
- Lidocaine Patches: Numb the affected area for temporary relief.
3. Physical and Complementary Therapies
- Physical Therapy: Exercises and stretches can improve circulation and alleviate muscle pain in the feet.
- Massage: Can improve blood flow and reduce discomfort.
- Acupuncture: May help manage chronic pain for some individuals.
- TENS (Transcutaneous Electrical Nerve Stimulation): A device that uses electrical impulses to reduce nerve pain.
4. Lifestyle Modifications
- Exercise Regularly: Low-impact activities like walking, swimming, or cycling improve circulation and overall nerve health.
- Dietary Changes: A balanced diet with controlled carbohydrate intake helps regulate blood sugar.
- Quit Smoking: Smoking impairs circulation, worsening nerve and foot health.
5. Preventative Foot Care
- Daily Foot Inspections:
- Check for blisters, cuts, ulcers, or color changes.
- Use a mirror or ask for help to examine the soles.
- Moisturize: Prevent dry, cracked skin with a gentle, non-perfumed lotion (avoid between the toes).
- Proper Footwear:
- Wear well-fitting, supportive shoes with soft insoles.
- Avoid tight socks or high heels that may worsen circulation or create pressure points.
- Routine Podiatrist Visits: Regular check-ups can help prevent complications like ulcers or infections.
6. Advanced Treatments for Severe Pain
- Nerve Blocks: Injections to numb specific nerves causing pain.
- Spinal Cord Stimulation: An implanted device delivers electrical impulses to disrupt pain signals.
- Alpha-Lipoic Acid: An antioxidant supplement that may reduce neuropathic pain in some cases (consult a doctor before use).
7. Treating Underlying Conditions
- Peripheral Artery Disease (PAD): If poor circulation contributes to foot pain, treatments like medication, angioplasty, or surgery may be necessary.
- Infections or Ulcers: Promptly treat wounds or infections with antibiotics and wound care to prevent complications.
8. Emotional and Psychological Support
- Chronic pain can lead to anxiety, depression, or stress. Joining support groups or seeking counseling can improve emotional well-being and pain management.
