What is Gabapentin ?
Gabapentin is used to help control partial seizures (convulsions) in the treatment of epilepsy. This medicine cannot cure epilepsy and will only work to control seizures for as long as you continue to take it.
Gabapentin is also used to manage a condition called postherpetic neuralgia, which is pain that occurs after shingles.
Gabapentin works in the brain to prevent seizures and relieve pain for certain conditions in the nervous system. It is not used for routine pain caused by minor injuries or arthritis. Gabapentin is an anticonvulsant.
This medicine is available only with your doctor’s prescription.
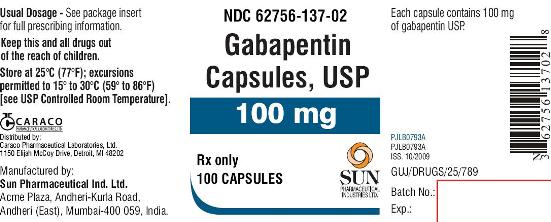
This product is available in the following dosage forms:
- Capsule
- Tablet
- Tablet, Extended Release, 24 HR
- Solution
- Suspension
Is Gabapentin Addictive ?
No. Gabapentin is not considered addictive.
But it is possible to develop a physical dependence on the drug. In fact, people can experience withdrawal symptoms for up to 45 days after they stop taking gabapentin. Although gabapentin does give some people a euphoric “high” which can cause gabapentin abuse, gabapentin abusers do not present with the kind of compulsive, drug-seeking behavior or strong cravings that indicates addiction.
Unfortunately, our clinical experience suggests that gabapentin is now prevalent as a drug of abuse. The drug’s effects vary with the user, dosage, past experience, psychiatric history, and expectations. Individuals describe varying experiences with gabapentin abuse, including: euphoria, improved sociability, a marijuana-like ‘high’, relaxation, and sense of calm, although not all reports are positive (for example, ‘zombie-like’ effects).
In primary care, an increasing number and urgency of prescription requests cannot necessarily be explained by the increased number of cases of neuropathic pain. In the substance misuse service, the numbers admitting to using gabapentin are also growing.
A 2007 report described the case of a 67-year-old woman with mood disorders and a history of alcohol abuse who was prescribed gabapentin (as well as naproxen and amitriptyline) for pain from polyneuritis. Owing to tolerance, she was prescribed 4800 mg/day (over the maximum recommended dose), but further escalated her intake to 7200 mg daily. She requested gabapentin without a prescription from pharmacists and visited numerous physicians, exaggerating her symptoms, to obtain the desired quantities.

When the patient was finally no longer able to obtain gabapentin through these methods, she developed withdrawal symptoms, characterized by trembling, sweating, excitation, pallor, and exophthalmia. The withdrawal required hospitalization, where a change to alternative pain control medications was made. Within several months, the patient had resumed abuse of gabapentin.
Another report described 3 cases of gabapentin-associated withdrawal symptoms after abrupt discontinuation of total daily doses of 4800 mg, 3600 mg, and 2400 mg.
Similar symptoms were reported in 2 patients with histories of alcohol abuse. The first case involved a 33-year-old man taking 3600 mg of gabapentin daily, which was twice his prescribed dose. He had been obtaining gabapentin refills early to reduce his craving for alcohol and make him feel calmer. When further refills were denied, he abruptly stopped taking the gabapentin and suffered acute withdrawal symptoms.
The second case described a 63-year-old man with a history of alcohol abuse who was taking gabapentin at 4900 mg/day instead of the prescribed 1800 mg/day. After presentation to the hospital and discontinuation of gabapentin, he developed severe withdrawal symptoms. Withdrawal symptoms in these patients included disorientation, confusion, tachycardia, diaphoresis, tremulousness, and agitation. The withdrawal symptoms resolved upon resumption of gabapentin.
The use of nonprescribed gabapentin by patients attending substance abuse clinics has also been reported.
A questionnaire-based survey completed by 129 respondents attending 6 substance abuse treatment clinics found that 22% of patients admitted to using nonprescribed gabapentin. As a comparison, nonprescribed use of pregabalin was 3%, benzodiazepines 47%, and cannabis 43%.
Some patients taking nonprescribed gabapentin reported using the drug to become intoxicated or to potentiate the effect of methadone.
