What is Fibromyalgia?
Fibromyalgia (fi·bro·my·al·gi·a) is a condition that causes pain all over the body (also referred to as widespread pain), sleep problems, fatigue, and often emotional and mental distress. People with fibromyalgia may be more sensitive to pain than people without fibromyalgia.
This is called abnormal pain perception processing. Fibromyalgia affects about 4 million US adults, about 2% of the adult population. The cause of fibromyalgia is not known, but it can be effectively treated and managed.
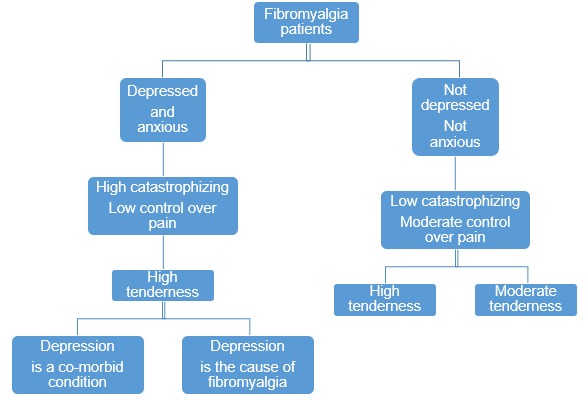
Fibromyalgia is a clinical entity characterized by the combination of ill-defined symptoms including chronic widespread pain, with concomitant fatigue, sleeping disorders and cognitive disturbances. The severity of these symptoms can vary significantly during the course of the disease. Fibromyalgia has been described as an arbitrarily created syndrome that lies at the extreme end of the spectrum of poly-symptomatic distress.
The term poly-symptomatic was used to emphasize the variety of multiple different symptoms that can be found in fibromyalgia patients, while the distress can have a physical and/or a psychological component. This exact nature of fibromyalgia makes it difficult to be clearly defined, often overlapping with disorders that are characterized by similar symptoms.
It is important to note that fibromyalgia is not an exclusion diagnosis as it can co-exist with other clinical conditions.
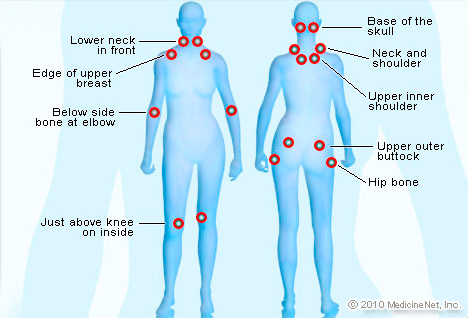
What are the Signs and Symptoms of Fibromyalgia?
The most common symptoms of fibromyalgia are
- Pain and stiffness all over the body
- Fatigue and tiredness
- Depression and anxiety
- Sleep problems
- Problems with thinking, memory, and concentration
- Headaches, including migraines
Other symptoms may include:
- Tingling or numbness in hands and feet
- Pain in the face or jaw, including disorders of the jaw known as temporomandibular joint syndrome (also known as TMJ)
- Digestive problems, such as abdominal pain, bloating, constipation, and even irritable bowel syndrome (also known as IBS)
Fibromyalgia is a disorder characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory and mood issues. Researchers believe that fibromyalgia amplifies painful sensations by affecting the way your brain processes pain signals.
Symptoms sometimes begin after a physical trauma, surgery, infection or significant psychological stress. In other cases, symptoms gradually accumulate over time with no single triggering event.
Women are much more likely to develop fibromyalgia than are men. Many people who have fibromyalgia also have tension headaches, temporomandibular joint (TMJ) disorders, irritable bowel syndrome, anxiety and depression.
While there is no cure for fibromyalgia, a variety of medications can help control symptoms. Exercise, relaxation and stress-reduction measures also may help.
In general, treatments for fibromyalgia include both medication and self-care. The emphasis is on minimizing symptoms and improving general health. No one treatment works for all symptoms.
What are the Risk factors for Fibromyalgia?
Known risk factors include:
- Age. Fibromyalgia can affect people of all ages, including children. However, most people are diagnosed during middle age and you are more likely to have fibromyalgia as you get older.
- Lupus or Rheumatoid Arthritis. If you have lupus or rheumatoid arthritis (RA), you are more likely to develop fibromyalgia.
Some other factors have been weakly associated with the onset of fibromyalgia, but more research is needed to see if they are real. These possible risk factors include:
- Sex. Women are twice as likely to have fibromyalgia as men.
- Stressful or traumatic events, such as car accidents, post-traumatic stress disorder (PTSD)
- Repetitive injuries. Injury from repetitive stress on a joint, such as frequent knee bending.
- Illness (such as viral infections)
- Family history
- Obesity
How is Fibromyalgia Diagnosed?
Doctors usually diagnose fibromyalgia using the patient’s history, physical examination, X-rays, and blood work.
How is Fibromyalgia Treated?
Fibromyalgia can be effectively treated and managed with medication and self-management strategies. You can learn about self-management strategies in the section below titled How can I improve my quality of life?
Fibromyalgia should be treated by a doctor or team of healthcare professionals who specialize in the treatment of fibromyalgia and other types of arthritis, called rheumatologists. Doctors usually treat fibromyalgia with a combination of treatments, which may include:
- Medications, including prescription drugs and over-the-counter pain relievers
- Aerobic exercise and muscle strengthening exercise
- Patient education classes, usually in primary care or community settings
- Stress management techniques such as meditation, yoga, and massage
- Good sleep habits to improve the quality of sleep
- Cognitive behavioral therapy (CBT) to treat underlying depression. CBT is a type of talk therapy meant to change the way people act or think
In addition to medical treatment, people can manage their fibromyalgia with the self-management strategies described below, which are proven to reduce pain and disability, so they can pursue the activities important to them.
What are the Complications of Fibromyalgia?
Fibromyalgia can cause pain, disability, and a lower quality of life. US adults with fibromyalgia may have complications such as:
- More hospitalizations. If you have fibromyalgia you are twice as likely to be hospitalized as someone without fibromyalgia.
- Lower quality of life. Women with fibromyalgia may experience a lower quality of life.
- Higher rates of major depression. Adults with fibromyalgia are more than 3 times more likely to have major depression than adults without fibromyalgia. Screening and treatment for depression are extremely important.
- Higher death rates from suicide and injuries. Death rates from suicide and injuries are higher among fibromyalgia patients, but overall mortality among adults with fibromyalgia is similar to the general population.
- Higher rates of other rheumatic conditions. Fibromyalgia often co-occurs with other types of arthritis such as osteoarthritis, rheumatoid arthritis, systemic lupus erythematosus, and ankylosing spondylitis.
How is Fibromyalgia Treated?
You and your doctor can treat fibromyalgia with medicines, lifestyle changes, and complementary therapy. However, fibromyalgia can be hard to treat. It’s important you find a doctor who is familiar with the disorder and its treatment.
Doctors may prescribe one or more of the following medicines to help treat the symptoms of fibromyalgia:
- Ibuprofen, aspirin, or naproxen you can buy over the counter.
- Narcotic medicines to treat severe pain.
- Duloxetine and minacipran to help the pain and fatigue.
- Pregabalin to help treat nerve pain.
Making lifestyle changes can also help you manage your fibromyalgia, including:
- Getting enough sleep.
- Exercising.
- Adjusting your work demands.
- Eating well.
You can also try complementary therapies such as:
- Massage therapy.
- Movement therapy.
- Chiropractic therapy.
- Acupuncture.
- Diet supplements.
If you are using or would like to try a complementary therapy you should speak with your doctor, who may know more about if it is safe to try.
Fibromyalgia Medications
Medications can help reduce the pain of fibromyalgia and improve sleep. Common choices include:
- Pain relievers. Over-the-counter pain relievers such as acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve, others) may be helpful. Your doctor might suggest a prescription pain reliever such as tramadol (Ultram, Conzip). Narcotics are not advised, because they can lead to dependence and may even worsen the pain over time.
- Antidepressants. Duloxetine (Cymbalta) and milnacipran (Savella) may help ease the pain and fatigue associated with fibromyalgia. Your doctor may prescribe amitriptyline at night to help promote sleep.
- Anti-seizure drugs. Medications designed to treat epilepsy are often useful in reducing certain types of pain. Gabapentin (Neurontin, Gralise) is sometimes helpful in reducing fibromyalgia symptoms, while pregabalin (Lyrica) was the first drug approved by the Food and Drug Administration to treat fibromyalgia.
Drugs associated with Fibromyalgia

How to Treat Fibromyalgia by Gabapentin ?
New research supported by the National Institutes of Health’s National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) shows that the anticonvulsant medication gabapentin, which is used for certain types of seizures, can be an effective treatment for the pain and other symptoms associated with the common, often hard-to-treat chronic pain disorder, fibromyalgia.

In the NIAMS-sponsored, randomized, double-blind clinical trial of 150 women (90 percent) and men with the condition, Lesley M. Arnold, M.D., director of the Women’s Health Research Program at the University of Cincinnati College of Medicine, and her colleagues found that those taking gabapentin at dosages of 1,200 to 2,400 mg daily for 12 weeks displayed significantly less pain than those taking placebo. Patients taking gabapentin also reported significantly better sleep and less fatigue. For the majority of participants, the drug was well tolerated. The most common side effects included dizziness and sedation, which were mild to moderate in severity in most cases.
NIAMS Director Stephen I. Katz. M.D., Ph.D., remarked that “While gabapentin does not have Food and Drug Administration approval for fibromyalgia1, I believe this study offers additional insight to physicians considering the drug for their fibromyalgia patients. Fibromyalgia is a debilitating condition for which current treatments are only modestly effective, so a study such as this is potentially good news for people with this common, painful condition.”
Fibromyalgia is a chronic disorder characterized by chronic, widespread muscle pain and tenderness, and is frequently accompanied by fatigue, insomnia, depression, and anxiety. It affects three million to six million Americans, mostly women, and can be disabling.
The precise cause of fibromyalgia in not known, but research suggests it is related to a problem with the central nervous system’s processing of pain. As with some other chronic pain conditions, people with fibromyalgia often develop a heightened response to stimuli, experiencing pain that would not cause problems in other people. Yet, unlike many other pain syndromes, there is no physical evidence of inflammation or central nervous system damage.
Although gabapentin has little, if any, effect on acute pain, it has shown a robust effect on pain caused by a heightened response to stimuli related to inflammation or nerve injury in animal models of chronic pain syndromes. Researchers have suspected that it might have the same effect in people with fibromyalgia. The new research, published in the April 2007 edition of Arthritis & Rheumatism, indicates the suspicions were correct.
Although the researchers cannot say with certainty how gabapentin helps reduce pain, Dr. Arnold says one possible explanation involves the binding of gabapentin to a specific subunit of voltage-gated calcium channels on neurons. “This binding reduces calcium flow into the nerve cell, which reduces the release of some signaling molecules involved in pain processing,” she says.
How gabapentin improves sleep and other symptoms is less clear, and there are probably different mechanisms involved in fibromyalgia symptoms. “Gabapentin improved sleep, which is an added benefit to patients with fibromyalgia who often report unrefreshing or disrupted sleep,” Dr. Arnold says.
What is important is that people with fibromyalgia now have a potential new treatment option for a condition with few effective treatments. “Studies like this give clinicians evidence-based information to guide their treatment of patients,” says Dr. Arnold.
Gabapentin Dosage for Fibromyalgia
Twenty-nine studies (3571 participants), studied gabapentin at daily doses of 1200 mg or more in 12 chronic pain conditions; 78% of participants were in studies of postherpetic neuralgia, painful diabetic neuropathy or mixed neuropathic pain. Using the IMMPACT definition of at least moderate benefit, gabapentin was superior to placebo in 14 studies with 2831 participants, 43% improving with gabapentin and 26% with placebo; the NNT was 5.8 (4.8 to 7.2). Using the IMMPACT definition of substantial benefit, gabapentin was superior to placebo in 13 studies with 2627 participants, 31% improving with gabapentin and 17% with placebo; the NNT was 6.8 (5.6 to 8.7). These estimates of efficacy are more conservative than those reported in a previous review. Data from few studies and participants were available for other painful conditions.
Adverse events occurred significantly more often with gabapentin. Persons taking gabapentin can expect to have at least one adverse event (66%), withdraw because of an adverse event (12%), suffer dizziness (21%), somnolence (16%), peripheral oedema (8%), and gait disturbance (9%). Serious adverse events (4%) were no more common than with placebo.
There were insufficient data for comparisons with other active treatments.
