Post-traumatic stress disorder (PTSD) is a real illness. You can get PTSD after living through or seeing a traumatic event, such as war, a hurricane, sexual assault, physical abuse, or a bad accident. PTSD makes you feel stressed and afraid after the danger is over. It affects your life and the people around you.
PTSD can cause problems like
- Flashbacks, or feeling like the event is happening again
- Trouble sleeping or nightmares
- Feeling alone
- Angry outbursts
- Feeling worried, guilty, or sad
PTSD starts at different times for different people. Signs of PTSD may start soon after a frightening event and then continue. Other people develop new or more severe signs months or even years later. PTSD can happen to anyone, even children.
Treatment may include talk therapy, medicines, or both. Treatment might take 6 to 12 weeks. For some people, it takes longer.
Certainly. Here’s a comprehensive and detailed explanation of Post-Traumatic Stress Disorder (PTSD) in English
What is Post-Traumatic Stress Disorder (PTSD)?
Post-Traumatic Stress Disorder (PTSD) is a mental health condition triggered by experiencing or witnessing a traumatic event. These events often involve actual or threatened death, serious injury, or sexual violence. While it is normal to feel distress immediately after trauma, PTSD involves long-lasting symptoms that interfere with daily life and do not go away with time.
1. Common Causes of PTSD
PTSD can develop after a wide range of traumatic experiences, including:
- Combat or war exposure
- Physical or sexual assault
- Childhood abuse or neglect
- Serious accidents (car crashes, industrial incidents)
- Natural disasters (earthquakes, floods, hurricanes)
- Sudden loss of a loved one
- Terrorist attacks
Not everyone who experiences trauma develops PTSD—genetics, support systems, coping mechanisms, and brain chemistry all play roles.
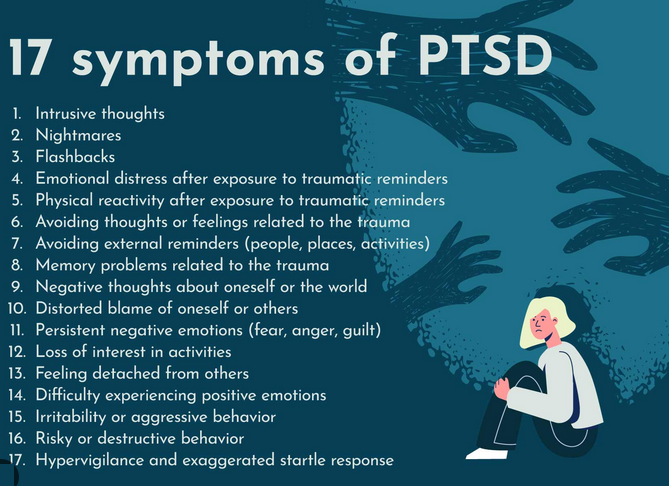
2. Core Symptoms of PTSD
PTSD symptoms fall into four categories, according to the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders):
A. Intrusion (Re-experiencing)
- Flashbacks – feeling like the trauma is happening again
- Nightmares or disturbing dreams about the event
- Intrusive thoughts or memories that pop up unexpectedly
- Emotional distress or physical reactions to reminders (triggers)
B. Avoidance
- Avoiding reminders (people, places, conversations, activities) of the trauma
- Avoiding thoughts, feelings, or conversations about the trauma
C. Negative Alterations in Cognition and Mood
- Persistent negative thoughts about oneself, others, or the world (“I’m broken,” “No one can be trusted”)
- Distorted blame of self or others
- Loss of interest in previously enjoyed activities
- Feeling detached or estranged from others
- Inability to experience positive emotions
D. Alterations in Arousal and Reactivity
- Hypervigilance – being constantly “on edge”
- Exaggerated startle response
- Irritability or angry outbursts
- Sleep disturbances (insomnia, trouble staying asleep)
- Difficulty concentrating
3. Duration and Onset
- Symptoms must last at least one month for a PTSD diagnosis.
- They can appear within weeks after the traumatic event or be delayed by months or even years.
4. Diagnosis Criteria (DSM-5)
To be diagnosed with PTSD, an individual must meet the following criteria:
| Category | Criteria |
|---|---|
| Exposure to trauma | Directly experienced, witnessed, or learned about traumatic event affecting close others |
| Re-experiencing symptoms | ≥1 symptom |
| Avoidance symptoms | ≥1 symptom |
| Negative thoughts/mood | ≥2 symptoms |
| Arousal/reactivity changes | ≥2 symptoms |
| Duration | More than 1 month |
| Functional impact | Causes significant distress or impairment |
5. Risk Factors
| Factor | Description |
|---|---|
| Previous trauma | Especially during childhood |
| Mental health history | Anxiety, depression, substance use |
| Lack of social support | Isolation increases vulnerability |
| Genetics and brain chemistry | Differences in stress hormone regulation and brain structures (e.g., amygdala, hippocampus) |
6. Biological Mechanism (Simplified)
- Trauma overactivates the brain’s fear system, especially the amygdala.
- The hippocampus, responsible for memory, may shrink, making it hard to distinguish past from present (causing flashbacks).
- Cortisol and adrenaline levels become dysregulated, keeping the body in a prolonged “fight-or-flight” mode.
- Neural circuits in emotion regulation and memory processing are altered.
7. Treatment Options
A. Psychotherapy (First-line treatment)
1. Cognitive Behavioral Therapy (CBT)
- Helps reframe negative thoughts and reduce avoidance
- May include Cognitive Processing Therapy (CPT) and Prolonged Exposure Therapy
2. Exposure Therapy
- Gradual, controlled confrontation with trauma-related memories or situations to desensitize emotional reactions
3. EMDR (Eye Movement Desensitization and Reprocessing)
- Combines trauma recall with guided eye movements to help reprocess traumatic memories
4. Trauma-Focused Therapy
- Specialized approaches for PTSD, often incorporating mindfulness, somatic awareness, or narrative exposure
B. Medications
| Medication Class | Examples | Purpose |
|---|---|---|
| SSRIs (first-line) | Sertraline, Paroxetine | Reduce depression, anxiety, intrusive thoughts |
| SNRIs | Venlafaxine | Alternative to SSRIs |
| Prazosin | — | Often used to treat PTSD-related nightmares |
| Antipsychotics / Mood stabilizers | — | Sometimes used in severe or treatment-resistant cases |
Benzodiazepines are not recommended long-term due to risk of dependence.
8. Complications and Co-Occurring Disorders
PTSD can coexist with or lead to:
- Depression
- Anxiety disorders
- Substance use disorder
- Suicidal thoughts or behaviors
- Chronic physical health conditions (e.g., high blood pressure, heart disease)
9. Prognosis
- With proper treatment, many people recover fully or significantly improve.
- Others may experience chronic PTSD, but symptoms can be managed effectively.
- Early intervention, strong social support, and consistent care improve outcomes.
10. How to Support Someone with PTSD
- Be patient and nonjudgmental
- Offer a safe space to talk (but don’t force them to discuss trauma)
- Encourage professional help
- Avoid triggers when possible
- Learn about PTSD to better understand their experience
Summary Table
| Aspect | Details |
|---|---|
| Cause | Exposure to trauma |
| Key Symptoms | Flashbacks, avoidance, negative mood, hyperarousal |
| Diagnosis | Based on DSM-5 criteria |
| Onset | Within weeks or delayed months/years |
| Treatment | Therapy (CBT, EMDR), SSRIs, Prazosin |
| Outlook | Treatable with professional intervention |
