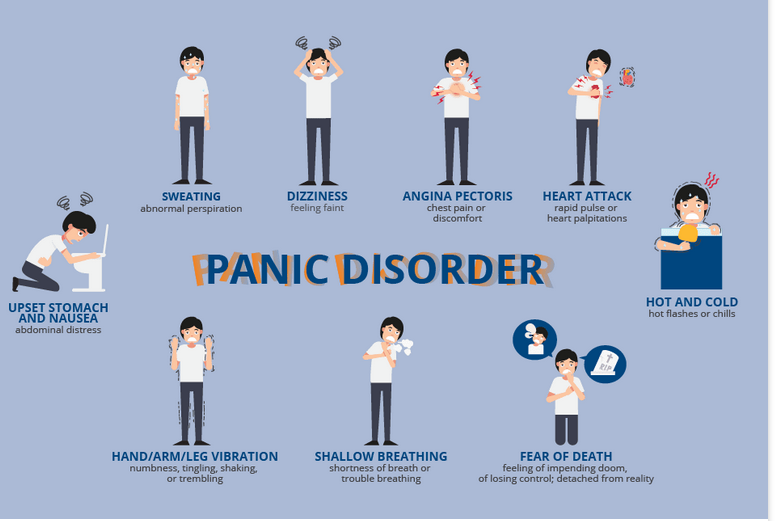
Panic disorder is a type of anxiety disorder. It causes panic attacks, which are sudden feelings of terror when there is no real danger. You may feel as if you are losing control. You may also have physical symptoms, such as
- Fast heartbeat
- Chest or stomach pain
- Breathing difficulty
- Weakness or dizziness
- Sweating
- Feeling hot or a cold chill
- Tingly or numb hands
Panic attacks can happen anytime, anywhere, and without warning. You may live in fear of another attack and may avoid places where you have had an attack. For some people, fear takes over their lives and they cannot leave their homes.
Panic disorder is more common in women than men. It usually starts when people are young adults. Sometimes it starts when a person is under a lot of stress. Most people get better with treatment. Therapy can show you how to recognize and change your thinking patterns before they lead to panic. Medicines can also help.
What is panic disorder?
If you have repeated, and unexpected panic attacks, you may have panic disorder. Panic disorder causes bouts of overwhelming fear when there is no specific cause for the fear. In between panic attacks, you may worry greatly about when and where the next one may happen. It can even keep you from leaving your home.
What causes panic disorder?
Panic disorder is a common mental health problem. It often starts in the teens or early adulthood, but may also begin in childhood. Women are twice as likely as men to have it. There may be a genetic link. It tends to run in families.
Panic disorder may be an overreaction of the body’s normal survival instincts and behaviors. In people with panic disorder, the body may be more sensitive to hormones that trigger excited feelings in the body.
What are the symptoms of panic disorder?
Panic attacks can happen in other types of anxiety disorders, too. Generally, if you have 4 or more panic attacks and if you always worry about having another, you have panic disorder. Symptoms of a panic attack may include:
- Pounding heart
- Sweating
- Trembling or shaking
- Shortness of breath
- Sense of choking
- Nausea or belly pain
- Dizziness or lightheadedness
- Feeling unreal or disconnected from oneself
- Fear of losing control
- Fear of “going crazy” or dying
- Numbness
- Chills or hot flashes
- Chest pain and other symptoms that mimic a heart attack
Panic disorder can be upsetting and disabling. An attack can last from a few minutes to an hour or sometimes longer.
The symptoms of a panic attack may look like other mental health conditions. Always see your healthcare provider for a diagnosis.
How is panic disorder diagnosed?
Your healthcare provider or a mental health professional may diagnose you with panic disorder based on your symptoms. Generally, if you have 4 or more panic attacks and if you are in constant fear of having another, you have panic disorder.
How is panic disorder treated?
Treatment may include:
- Anti-anxiety and antidepressant medications
- Counseling, such as cognitive behavioral therapy
The Detail Medication Listing for Panic Disorder
Panic Disorder is characterized by recurrent unexpected panic attacks and ongoing fear of having more attacks. Medication is often used when attacks are frequent, severe, or significantly impairing.
Here is a detailed medication listing specifically for Panic Disorder, including commonly prescribed drugs, their mechanisms, pros and cons, and when they are typically used.
1. Selective Serotonin Reuptake Inhibitors (SSRIs)
First-line medications for long-term treatment
Common SSRIs:
- Sertraline (Zoloft)
- Paroxetine (Paxil)
- Fluoxetine (Prozac)
- Escitalopram (Lexapro)
Why used: Most evidence-based for panic disorder; reduce frequency and intensity of panic attacks.
Pros:
- Effective for long-term control.
- Lower risk of abuse.
- Also treat comorbid depression/anxiety.
Cons:
- Takes 2–6 weeks to work.
- May cause temporary increase in anxiety during first 1–2 weeks.
- Side effects: nausea, insomnia, sexual dysfunction, headache.
2. Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
Alternative first-line or second-line
Common SNRIs:
-
Venlafaxine XR (Effexor XR)
Why used: Shown effective in panic disorder; especially useful if other anxiety or depressive symptoms present.
Pros:
-
Also treats GAD and depression.
-
Fewer sexual side effects than SSRIs (in some cases).
Cons:
-
May raise blood pressure at high doses.
-
Discontinuation syndrome if missed doses.
3. Benzodiazepines
Used for rapid, short-term relief or in severe cases
Common Benzodiazepines:
-
Alprazolam (Xanax)
-
Clonazepam (Klonopin)
-
Lorazepam (Ativan)
Why used: Rapid onset; helpful for acute panic attacks or while waiting for antidepressants to work.
Pros:
-
Fast-acting (minutes).
-
Reduces physical symptoms like palpitations, tremors.
Cons:
-
Risk of dependence and tolerance.
-
Withdrawal can trigger panic-like symptoms.
-
Sedation, impaired cognition and coordination.
-
Not ideal for long-term use.
Note: Sometimes used as a temporary add-on during SSRI initiation.
4. Tricyclic Antidepressants (TCAs)
Second-line option when SSRIs are not effective or tolerated
Common TCAs:
-
Imipramine
-
Clomipramine
Why used: Proven efficacy in panic disorder.
Pros:
-
Strong clinical data support.
-
Can work in treatment-resistant cases.
Cons:
-
More side effects: dry mouth, constipation, dizziness, weight gain.
-
Risk of overdose toxicity.
5. Monoamine Oxidase Inhibitors (MAOIs)
Third-line or treatment-resistant cases
Common MAOIs:
-
Phenelzine (Nardil)
-
Tranylcypromine (Parnate)
Why used: Highly effective in some treatment-resistant panic disorder cases.
Pros:
-
Strong efficacy in specific patients.
Cons:
-
Dietary restrictions (tyramine-free diet required).
-
Drug interactions.
-
Rarely used due to complexity and risk.
6. Others / Adjunctive Treatments
Buspirone:
-
Not effective for panic disorder. More useful in generalized anxiety.
Beta Blockers:
-
Propranolol may help physical symptoms of anxiety but not true panic attacks.
Atypical Antipsychotics (e.g. quetiapine):
-
Occasionally used as adjuncts in treatment-resistant panic disorder, but not first-line.
- ✅ Medication Strategy Summary for Panic Disorder
| Medication Class | Example | Use Level | Main Role |
|---|---|---|---|
| SSRIs | Sertraline | First-line | Long-term control |
| SNRIs | Venlafaxine XR | First/Second | Alternative if SSRI not tolerated |
| Benzodiazepines | Clonazepam | Short-term | Acute symptom relief |
| TCAs | Imipramine | Second-line | If SSRI fails or intolerable |
| MAOIs | Phenelzine | Third-line | Severe, resistant cases |
Treatment for panic disorders
Treatment for panic disorders is usually quite effective. Treatment will help you learn to recognize that the symptoms are not life-threatening. You will also learn coping skills and ways to relax to decrease the intensity and length of the panic attack.
- Would you like this list tailored by age group, comorbidities, or drug side-effect profiles?
- What are the complications of panic disorder?
- As the panic gets worse and an attacks last longer, you may find it very tough to cope with everyday life, keep a job, or function in social settings. You may fear going into places where it may be hard to escape or you feel trapped. Some people can’t leave their home for fear that help is not available or that he or she will be forced into a situation that will trigger an attack.
- People with this condition may also abuse alcohol or drugs to relieve stress.
- Key points about panic disorder
- Panic disorder is an overreaction of fear and anxiety to daily life stressors.
- The reaction causes a hyperphysical response, followed by intense worry that another attack will happen soon. This can upset the ability to function normally.
- It is a common disorder and can often lead to depression.
- Panic disorders can be disabling because you become so afraid of when the next panic attack may happen that you can’t cope with regular tasks.
- Treatment involves use of anti-anxiety medicines and antidepressants along with cognitive behavioral therapy.
- Next steps
- Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
