Diabetic neuropathy is a type of nerve damage caused by prolonged high blood sugar levels and is one of the most common complications of diabetes. Prevention and treatment focus on managing blood sugar levels, alleviating symptoms, and slowing the progression of nerve damage.
- Foot pain is common in people who have diabetes. It’s commonly caused by damage to the nerves and called diabetic neuropathy.
- Well-managed blood sugar levels can lower the risk of developing diabetic foot pain. Smoking cessation can help lower the risk too.
- Regular foot checks and exams are important for everyone with diabetes. Foot checks can help you avoid complications like foot ulcers and foot injuries.
Diabetes can impact almost every part of the body. Your legs, feet, and even toes are no exception. Many people with diabetes experience diabetes-related foot pain (also called diabetic foot neuropathy). The longer you have diabetes and the higher your blood sugar levels run, the more likely it is you’ll develop foot pain or discomfort in the future.
Diabetic Peripheral Neuropathy (DPN) is a type of nerve damage that can occur in people with diabetes. High blood sugar levels can injure nerves throughout your body, but DPN most often damages nerves in your legs and feet. Symptoms of DPN can range from pain and numbness to severe complications, such as foot ulcers and infections.


Peripheral neuropathy is nerve damage caused by chronically high blood sugar and diabetes. It leads to numbness, loss of sensation, and sometimes pain in your feet, legs, or hands. It is the most common complication of diabetes.
About 60% to 70% of all people with diabetes will eventually develop peripheral neuropathy, although not all suffer pain. Yet this nerve damage is not inevitable. Studies have shown that people with diabetes can reduce their risk of developing nerve damage by keeping theirblood sugar levels as close to normal as possible.
What causes peripheral neuropathy? Chronically high blood sugar levels damage nerves not only in your extremities but also in other parts of your body. These damaged nerves cannot effectively carry messages between the brain and other parts of the body.
This means you may not feel heat, cold, or pain in your feet, legs, or hands. If you get a cut or sore on your foot, you may not know it, which is why it’s so important to inspect your feet daily. If a shoe doesn’t fit properly, you could even develop a foot ulcer and not know it.
The consequences can be life-threatening. An infection that won’t heal because of poor blood flow causes risk for developing ulcers and can lead to amputation, even death.
This nerve damage shows itself differently in each person. Some people feel tingling, then later feel pain. Other people lose the feeling in fingers and toes; they have numbness. These changes happen slowly over a period of years, so you might not even notice it.
Because the changes are subtle and happen as people get older, people tend to ignore the signs of nerve damage, thinking it’s just part of getting older.
But there are treatments that can help slow the progression of this condition and limit the damage. Talk to your doctors about what your options are, and don’t ignore the signs because with time, it can get worse.
Drugs associated with Diabetic Peripheral Neuropathy

Why Gabapentin is Effective for Diabetic Neuropathy ?
Gabapentin is commonly prescribed for diabetic neuropathy due to its effectiveness in managing nerve pain. Here’s why it works well:
Mechanism of Action
- Gabapentin binds to the α2δ subunit of voltage-gated calcium channels in nerve cells, reducing calcium influx and decreasing the release of excitatory neurotransmitters (e.g., glutamate).
- This reduces the hyperexcitability of damaged nerves, alleviating pain.
Benefits for Diabetic Neuropathy
- Pain Relief: Gabapentin helps reduce burning, tingling, or shooting pain typical of diabetic neuropathy.
- Improved Sleep: Its sedative effects can help those whose pain disrupts sleep.
- Well-Tolerated: Gabapentin has a lower risk of addiction compared to opioid medications.
What are some risks of diabetic foot pain if you don’t get treatment?
Diabetes-related foot pain is more than just pain; it’s a warning sign from your body. This type of nerve pain can lead to other foot complications like:
- Dry, cracked skin: This may not sound too bad, but when your skin is too dry, your risk of getting skin infections goes up.
- Calluses: This is an area of thickened skin that has less feeling. People with diabetes get calluses faster and more often than those without diabetes.
- Ulcers: These are foot sores that develop due to poor blood circulation. All ulcers (no matter how small) need to be treated. Without treatment, they can become infected.
- Amputations: Foot infections can cause the skin and muscle tissues to die. Once this happens, it can’t be fixed. The only way to stop the infection from spreading to the rest of the body is to amputate part (or sometimes all) of the foot.
Diabetes-related foot pain can’t be cured. But treatment can keep it from getting worse. The best way to prevent or manage diabetic foot pain is by keeping your blood sugar in a healthy range. You can do this with the right diet, exercise, and diabetes medications.
Here are six things you can do at home to help manage your diabetes-related foot pain and prevent complications.
1. Check your feet
Check the bottoms of your feet every morning when you wake up and every night before you go to bed. Look for cuts, wounds, and anything else unusual.
2. Wear shoes around the house
When you have diabetic foot pain, you can’t always feel when you step on things. Wearing shoes helps to prevent cuts and injuries.
3. Follow up with your healthcare provider
It’s important to attend your regular healthcare appointments. Not only will your provider be able to perform foot exams, but they can catch problems early and keep them from becoming more serious.
4. Follow your diet plan
Just because diabetes-related foot pain isn’t reversible doesn’t mean it can’t be improved. The right diet helps keep blood sugar levels within a healthy range. You can work with a diabetes dietician to develop the right meal plans for you.
5. Stop smoking
Smoking damages your blood vessels and can worsen peripheral artery disease. Smoking cessation helps to improve blood flow to your feet.
If you’re having trouble quitting smoking, talk with your primary care provider or diabetes treatment team. They can recommend treatments and support groups that are right for you.
6. Have corns and calluses removed by a professional
Corns and calluses are areas of thickened skin that are less able to perceive pain and sensation. Treatment can help smooth these surfaces so that you can maintain better sensation in those areas. But don’t try to remove them on your own. This can lead to serious infections. Instead, work with a foot doctor (podiatrist) who is trained to care for people with diabetes.
Prevention of Diabetic Neuropathy
Blood Sugar Control
- Maintain blood sugar within target ranges to prevent nerve damage.
- Regularly monitor glucose levels as advised by your healthcare provider.
- A1C (average blood sugar over 3 months) should generally be kept below 7%, though individual targets may vary.
Healthy Lifestyle
- Diet: Follow a balanced diet rich in whole grains, lean proteins, healthy fats, and vegetables. Minimize sugary and processed foods.
- Exercise: Engage in regular physical activity, such as walking, swimming, or cycling, which improves circulation and helps control blood sugar.
- Weight Management: Maintaining a healthy weight reduces the risk of complications.
Routine Foot Care
- Inspect feet daily for sores, blisters, cuts, or changes in skin color or texture.
- Wear properly fitting shoes to prevent pressure sores or injuries.
- Moisturize skin to avoid dryness and cracking.
Control of Other Risk Factors
- Manage blood pressure and cholesterol to improve overall vascular health.
- Avoid smoking, as it impairs circulation and increases the risk of nerve damage.
What are treatment options for diabetic foot pain?
You can also take medication to help lessen symptoms from your diabetes-related foot pain. Here are some of the most commonly recommended ones:
- Pregabalin (Lyrica)
- Duloxetine (Cymbalta)
- Gabapentin (Neurontin)
- Amitriptyline (Elavil)
Over-the-counter pain relievers like acetaminophen (Tylenol), ibuprofen (Motrin, Advil), and naproxen (Aleve) don’t improve nerve pain.
Gabapentin for Diabetic Peripheral Neuropathy
Gabapentin is an anticonvulsant medication that is also used to treat nerve pain. Here’s how it relates to DPN:
Mechanism of Action:
Gabapentin works by modulating the activity of neurotransmitters and decreasing abnormal excitement in the brain. It is thought to inhibit the release of excitatory neurotransmitters, which can help alleviate pain.
Efficacy:
Several studies have demonstrated that gabapentin can be effective in reducing the pain associated with DPN. It is often used when other pain management strategies have not provided sufficient relief.
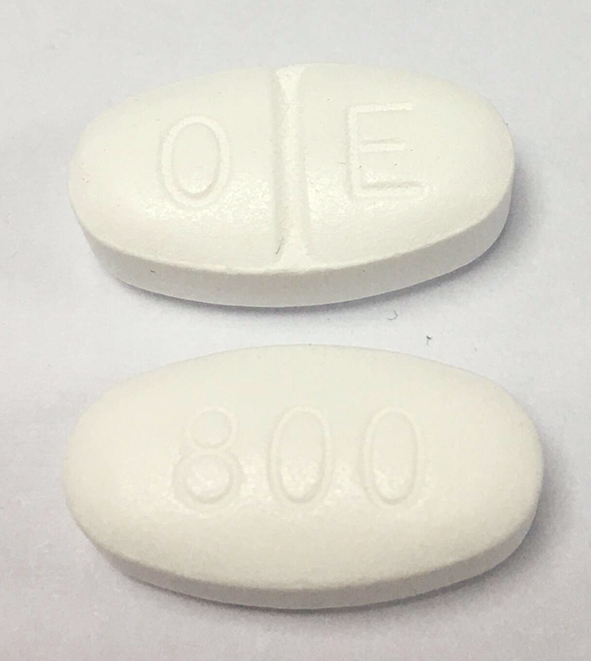
Dosage:
The typical starting dose for gabapentin in treating neuropathic pain is 300 mg per day, which can be gradually increased based on the patient’s response and tolerability. The maximum dose can go up to 3600 mg per day, divided into three doses.
Side Effects:
Common side effects of gabapentin include:
- Dizziness
- Drowsiness
- Fatigue
- Peripheral edema (swelling in the extremities)
- Weight gain
Less common but more severe side effects can include mood changes, difficulty with coordination, and severe allergic reactions.
Considerations:
- Gabapentin needs to be used with caution in elderly patients or those with kidney impairment, as it is excreted through the kidneys.
- It is important to monitor for any signs of abuse or dependence, as there is potential for misuse.
Management of Diabetic Peripheral Neuropathy
In addition to pharmacologic treatments like gabapentin, managing DPN involves a comprehensive approach:
- Blood Sugar Control:
- Maintaining good glycemic control is critical to prevent further nerve damage.
- Lifestyle Modifications:
- Regular exercise, a healthy diet, and smoking cessation can help manage symptoms.
- Foot Care:
- Regular foot inspections and proper foot care are essential to prevent complications like ulcers and infections.
- Other Medications:
- Other medications for DPN may include antidepressants (e.g., amitriptyline, duloxetine) and other anticonvulsants (e.g., pregabalin).
- Pain Management Strategies:
- Physical therapy, topical treatments, and alternative therapies (such as acupuncture) may also provide relief.